Background: Mortality review, well-documented in the medical literature, is a standardized process used to identify patient safety improvement opportunities and also to evaluate providers. As patient safety experts, hospitalists often review mortality cases for their hospitalist group or hospital. As the volume of cases is often not trivial, it can be difficult to allocate the appropriate time to evaluate all cases in detail. In order to improve the yield of review, cases need to be stratified for likelihood of identifying an improvement opportunity.
Purpose: The aim of the project is the development of a systematic method to review mortality cases leading to a high-yield identification of quality improvement opportunities for hospital medicine providers.
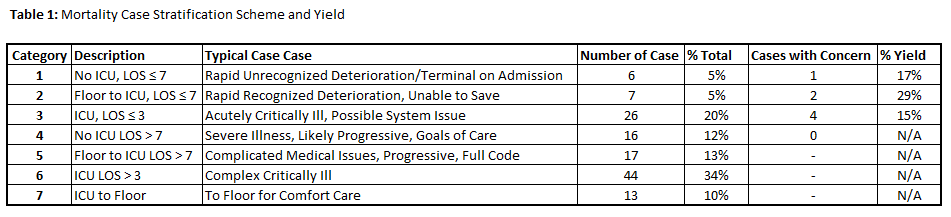
Description: The project was carried out in a 660-bed urban, academic, tertiary referral center. The initial pool of cases reviewed encompassed all deaths in the hospital on any service line within the Department of Medicine, including the medical intensive care unit, specialty floors and general medicine floors. Each mortality report provided information on admitting service, discharging service, length of stay, primary discharge diagnosis, and expected mortality. Reviews were completed by senior hospital medicine physicians with prior experience in case review. Initially all mortality cases were reviewed on monthly intervals, requiring 2-3 full days of effort, and reported out to a larger committee. The first elements of stratification were based on length of stay and expected mortality; however, expected mortality did not actually correlate on illness severity as it was dependent on provider documentation. After multiple improvement cycles, a stratification system based on length of stay, admitting, and discharging services, with a focus on level service change, such as floor to intensive care,was implemented (Table 1). A formal sample of 129 cases was stratified, with 55 falling in the high need for review categories (1-4). Cases with high likelihood of intensive care issues were deferred, as unlikely to have high-yield related specifically to hospital medicine. The review category classified by a length of stay of 7 days or less and being admitted to the floor, then transferred to the intensive care unit had the highest case yield at 29%, but only represented 5% of the total population (Table 1).
Conclusions: Stratifying mortality cases by length of stay and level of service change can help to find cases with a high likelihood of containing improvement opportunities. Identifying stratification features requires a high volume of case review and may be unique to the workflows and patient populations of each institution.