Background:
Clinicians rely on physiologic monitor alarms to notify them of their patients’ changing vital signs. Currently, alarms occur very frequently and usually do not warrant clinical intervention. High alarm burden can lead to alarm fatigue, often observed as a slower response or unintentional ignoring of clinically important alarms. For this reason, alarm fatigue has been frequently named a threat to patient safety by The Joint Commission. We aimed to critically examine the available literature on alarm fatigue.
Methods:
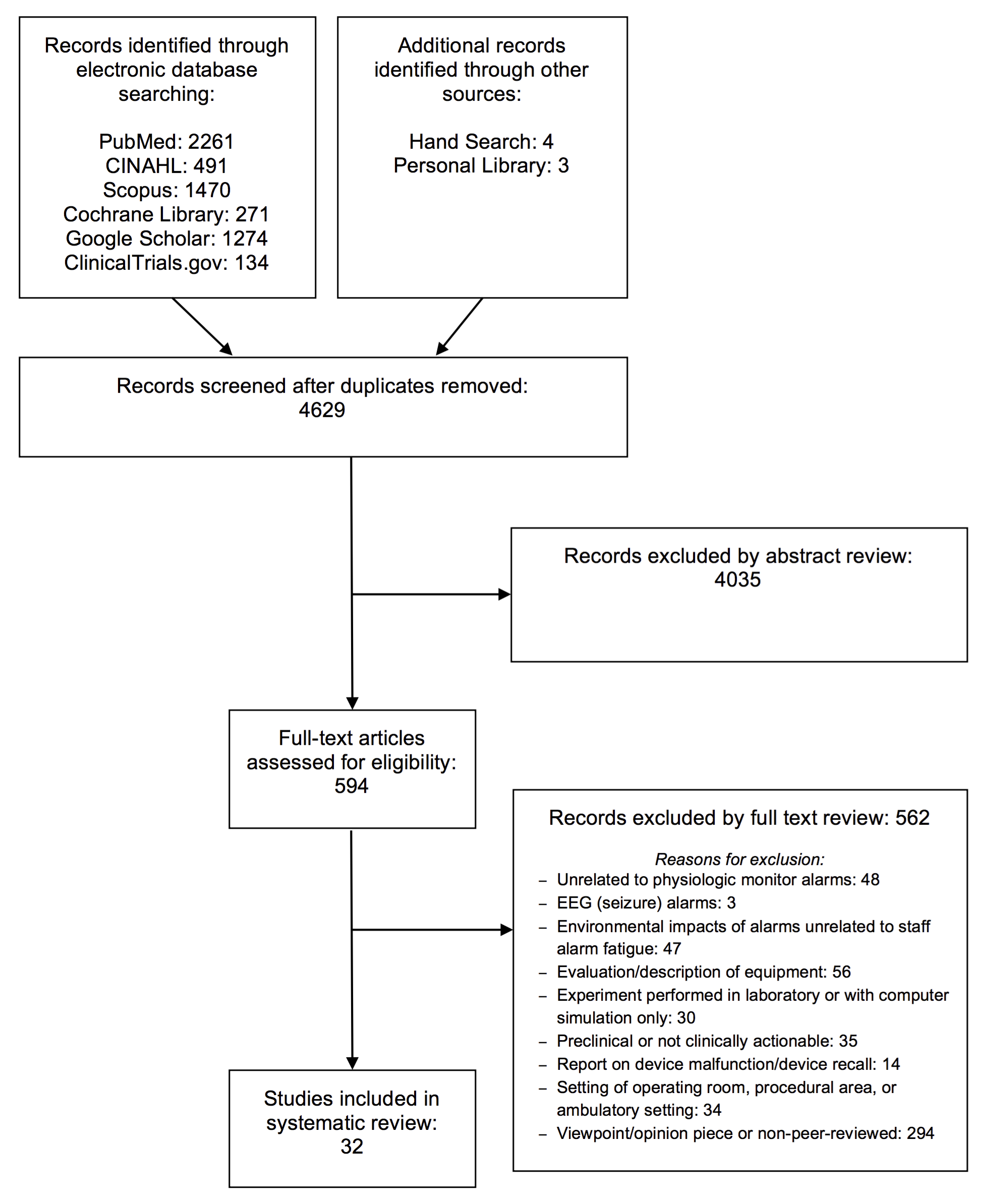
We performed a systematic review of the literature in accordance with the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines. We selected articles focused on hospital physiologic monitor alarms addressing any of the following: 1) the proportion of alarms that are actionable (defined as warranting a clinical intervention), 2) the relationship between alarm exposure and nurse response time, and 3) the effectiveness of interventions in reducing alarm frequency.
Results:
Our review produced 24 observational studies focused on alarm characteristics and response time along with 8 studies evaluating interventions. Actionable alarm proportions ranged from <1% to 36% across a variety of hospital settings. Two studies showed a relationship between high alarm exposure and longer nurse response time. Most intervention studies included multiple components implemented simultaneously. While studies varied widely in methodology, promising yet still unproven interventions included widening alarm parameters, instituting alarm delays, and using disposable electrocardiographic wires or frequently changed electrocardiographic electrodes.
Conclusions:
Physiologic monitor alarms are commonly nonactionable, and evidence supporting the concept of alarm fatigue is emerging. Several interventions have the potential to reduce alarms safely, but more rigorously designed studies with attention to safety and unintended adverse consequences are needed.