Background: The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) is a post-discharge survey which captures patient experience during and after hospitalization (1). Previous studies have demonstrated that high quality discharge communication is vital for patient safety, with poor communication leading to decreased medication adherence, unplanned readmissions, and poorer health outcomes—important implications for both patients and hospital systems (2,3). We examined low “Understanding Your Care” HCAHPS scores from patients discharged from hospital medicine services from our institution.
Purpose: Our project focused on understanding barriers to patients’ understanding of their health and medications at the time of discharge to target interventions. This project was designed by four medical students as part of University of Colorado’s Health Innovations Scholars Program in August 2023.
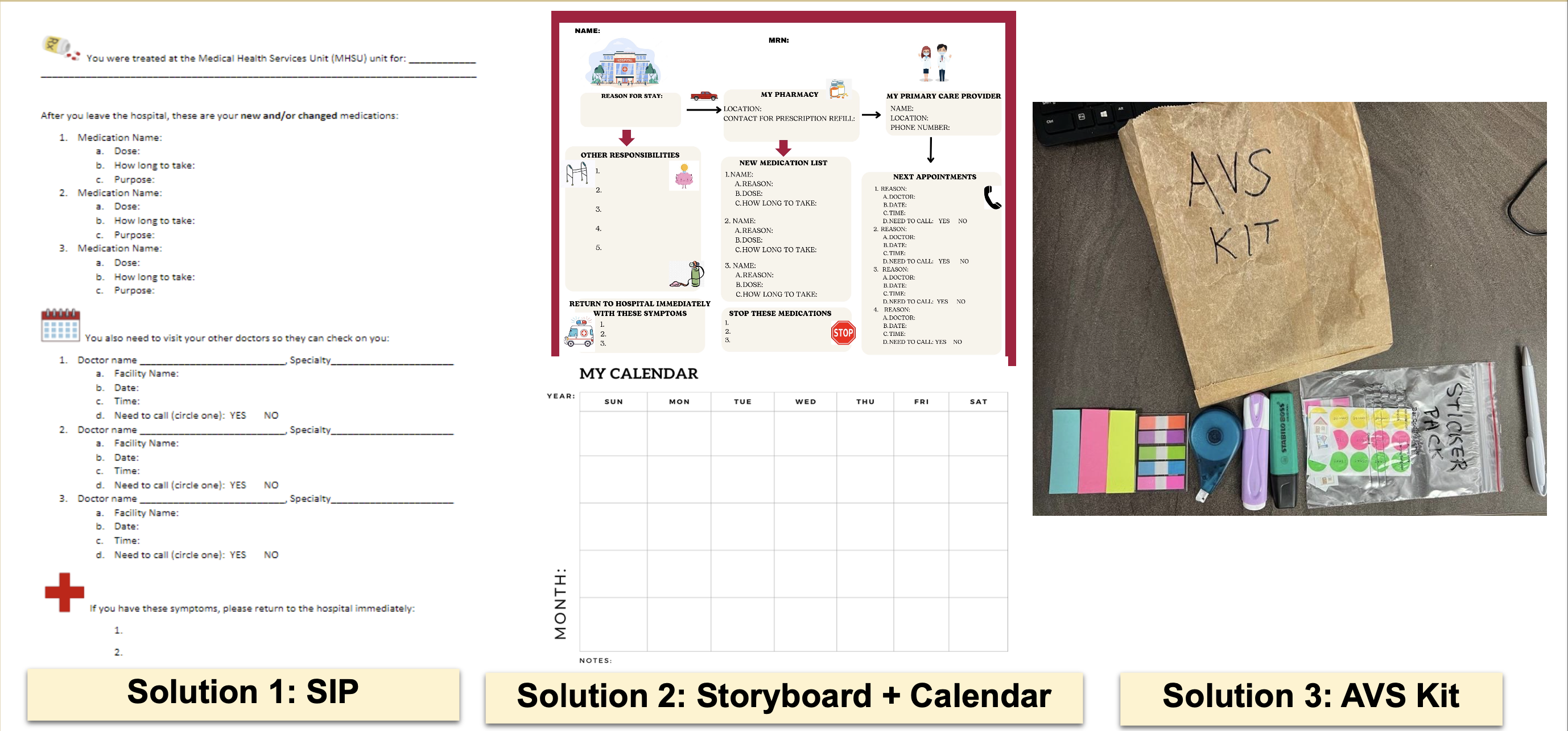
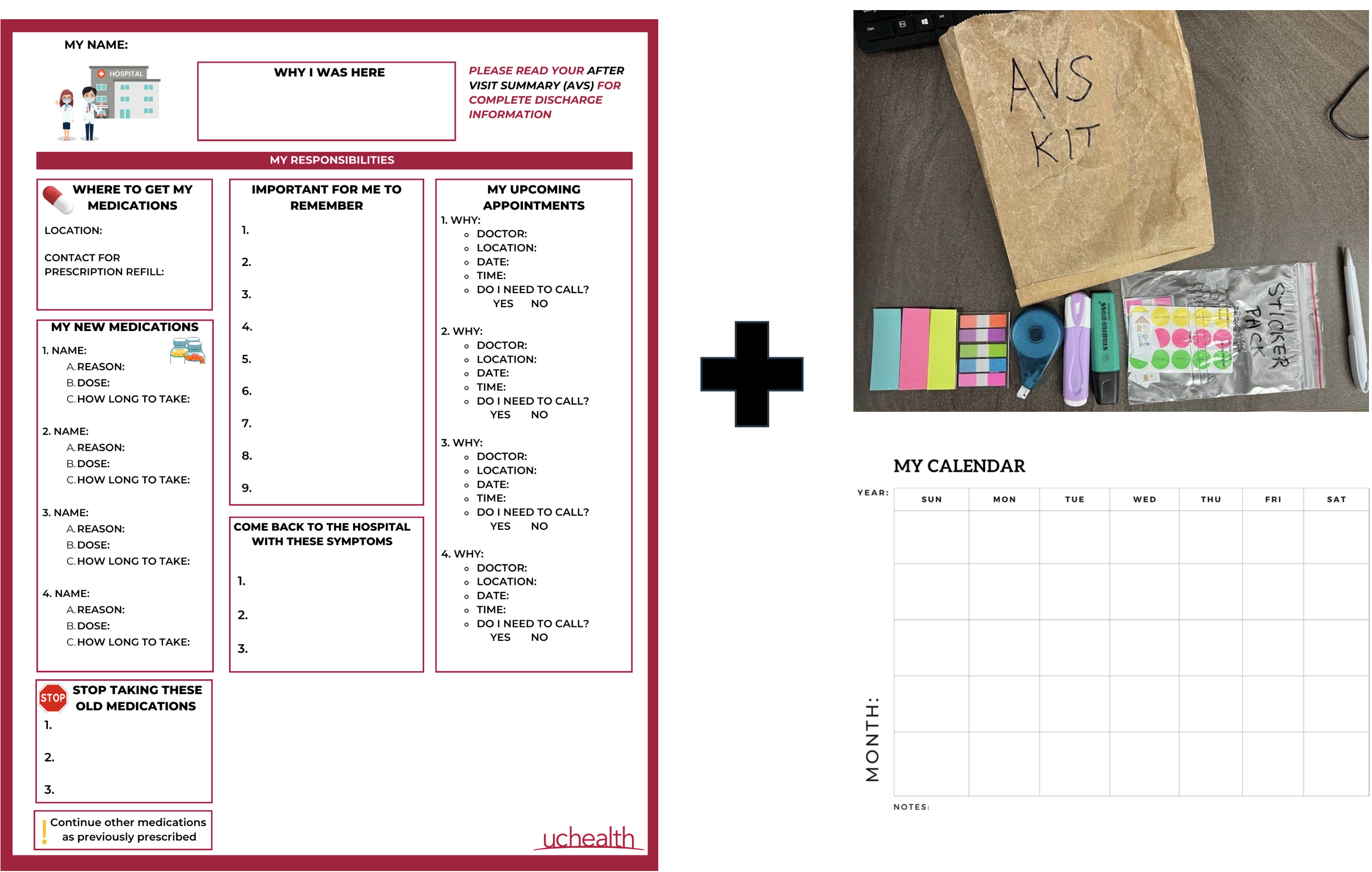
Description: We addressed two HCAHPS questions. The first was, “When I left the hospital, I had a good understanding of the things I was responsible for in managing my health.” The second was, “When I left the hospital, I clearly understood the purpose for taking each of my medications.” We started by conducting interviews with patients, clinicians, and discharge nurses to better understand discharge experiences. We discovered that each patient receives a standardized discharge packet but the discharge process itself was time-pressured, disjointed, and contained large amounts of information which was passively delivered to the patient. We also found a mismatch between patient reported confidence, which was high, and knowledge in managing their own health, which was lower. We hypothesized that increasing patient interaction and engagement during the discharge process could help increase knowledge retention and confidence among patients. Utilizing design thinking, we created three solution prototypes (Figure 1). Solution one, a simplified information page (SIP), was adapted from a published quality improvement project (4) and highlighted the most important discharge information; it also encouraged active learning by utilizing patient notetaking. Solution two was a combination of a graphic storyboard and calendar for post-discharge appointments. Solution three was a discharge kit, including stationery and stickers, which allowed the patient to interact directly with the standardized discharge instructions. Nurses and patients were then asked to provide feedback on the prototypes. Patients felt like the SIP was test-like and complicated. They were enthusiastic about the graphic storyboard organization but felt that it had too many components. The discharge kit was well-received by patients and nurses, and nurses noted potential benefits for patients who are less engaged or have lower health literacy. Based on this feedback, we designed a final simplified version of the storyboard with fewer graphics and kept the discharge kit (Figure 2), which was being actively utilized at the time of our program conclusion.
Conclusions: Our project identified that patients don’t have a clear understanding of their health at time of discharge. Using design thinking, we produced low-cost prototypes that yielded rich and rapid feedback on workflow considerate and patient-centered solutions with the potential to increase patient engagement and empower active involvement during the discharge process.