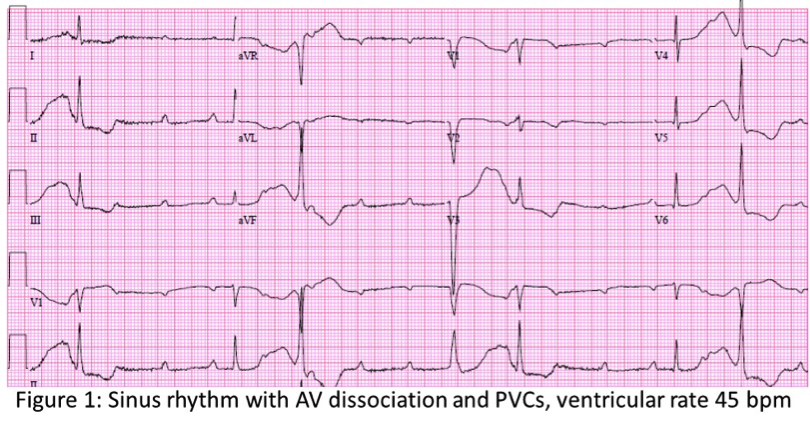
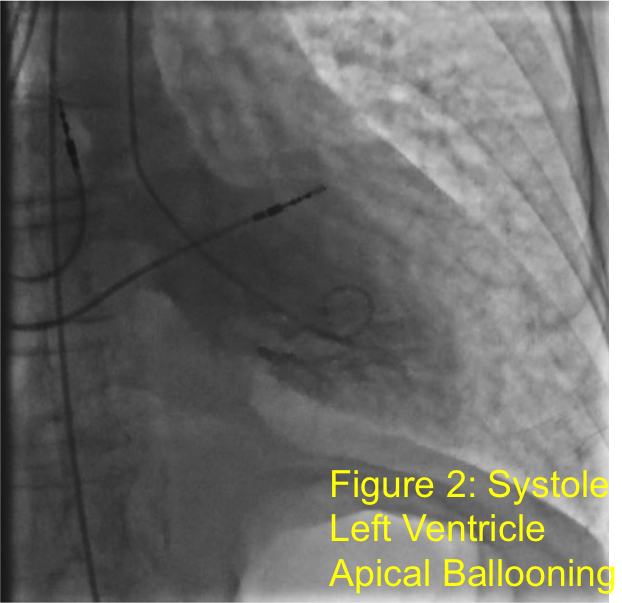
Case Presentation: Patient is a 71 year old female with hypertension and chronic obstructive pulmonary disease who presented after syncopal episodes and falls. She denied chest pain but did have lightheadedness and shortness of breath (SOB). She was started on transcutaneous pacing by EMS due to severe bradycardia. Admission EKG (fig 1) showed 3rd degree atrioventricular (AV) block and NSTEMI with troponin of 0.97 ng/mL. She was treated with Atropine and Cardiology implanted a pacemaker. First transthoracic echocardiogram (TTE) showed normal left ventricular function, but a few days later, she developed acute SOB due to pulmonary edema and heart failure. Second TTE showed hypokinesis and decreased ejection fraction from 55% to 20% (LVEF). Cardiac catherization showed diffuse small coronary vessels but no discrete culprit lesions and left ventricle apical ballooning (fig 2). She was diagnosed with Takotsubo Cardiomyopathy (TC) and further treatment included mechanical ventilation, hemodialysis, Milrinone drip and intra-aortic balloon pump. Subsequent TTE showed improvement in LVEF to 45%. She was discharged on Propranolol and Lisinopril but she returned promptly for respiratory distress requiring one more day of mechanical ventilation. CT chest showed bilateral pleural effusions requiring diuresis. Interestingly, on admission, thyroid stimulating hormone (TSH) was noted to be 0.256 mIU/L (0.34-5.60) with free T4 of 1.53 ng/dL (0.70-1.50). On re-admission, her TSH was 0.054 mIU/L and free T4 was 2.45 ng/dL. Thyroid Stimulating Immunoglobulin (TSI) level was < 0.10 IU/L (0.00-0.55). Thyroid Ultrasound was negative for nodules and she was started on Methimazole for thyrotoxicosis.
Discussion: Takotsubo cardiomyopathy (TC), also known as “stress cardiomyopathy”, is a transient systolic dysfunction of the apical or mid segments of the left ventricle. In this case, the patient met all Mayo Clinic diagnostic criteria, including reversible LV dysfunction, exclusion of obstructive coronary artery disease, elevated troponin, and absence of pheochromocytoma. Furthermore, the patient presented with complete AV heart block and thyrotoxicosis. Although several theories exist, TC is most frequently attributed to sympathetic hyperactivity via catecholamine excess. This is consistent with thyrotoxicosis since it causes exaggerated chronotropic and inotropic responses to catecholamines through upregulation of beta-adrenergic receptors in the heart. AV block is also a very rare occurrence with TC and the pathology is not well understood but one theory is that diffuse spasms in small branches of the coronary arteries may cause conduction disturbances. Hence, her thyrotoxicosis may be related to the AV block through inotropic, chronotropic, and dromotropic effects that impair AV conduction.
Conclusions: The treatment of TC is largely supportive with aspirin, beta-blockers and ACE inhibitors. However, early recognition of TC can affect decisions to avoid fibrinolytic therapy, use IV pressor support versus intra-aortic balloon pump and anticipate arrhythmias. Although the TSI was low, TSI is positive in only 50-70% of Graves’ disease. Since the patient had pre-existing subclinical hyperthyroidism, it is possible the TC and AV block may be related to thyrotoxicosis. Furthermore, repeating thyroid function tests may be useful as in this case where her thyrotoxicosis was more evident later on. If the patient is found to have Graves’ disease, then her TC and AV block may potentially be reversible.