Background: Point-of-Care Ultrasound (POCUS) is becoming an increasingly valuable tool in Internal Medicine. With the proper training, POCUS can provide insight into diagnostic dilemmas, resulting in expedited management and enhancing patient care. However, the ability to effectively utilize POCUS is directly related to the extent of each individual’s training. It is therefore critical to implement POCUS training within Internal Medicine residency education in order to adequately prepare the next generation of physicians to practice modern medicine. Yet, having limited faculty who are POCUS trained themselves provides a barrier to implementing such a curriculum.
Purpose: To overcome the above obstacle, we implemented a “Teach the Teacher” model as the foundation for the POCUS curriculum at Wake Forest Baptist Medical Center (WFBMC).
Description: WFMBC is a tertiary referral hospital with over 100 internal medicine house staff. In the first phase of the “Teach the Teacher” model, twenty Internal Medicine residents were selected to be POCUS Champions (PCs) to receive early training from the program faculty. PCs are initially students that develop into instructors and become advocates for future trainees. Training consists of structured lectures on heart, lung, and IVC anatomy, followed by hands on POCUS workshops with standardized patients. In the second phase, two resident PCs perform “gel rounds” with a POCUS trained faculty member during which exams are performed on patients in the hospital. The faculty supervisor assesses each resident’s understanding of basic ultrasound operation, image acquisition, and ability to properly perform each exam, while providing additional guidance when needed. Gel rounds continue until POCUS Champions can perform at least 25 acceptable heart, lung, and IVC exams under direct supervision.
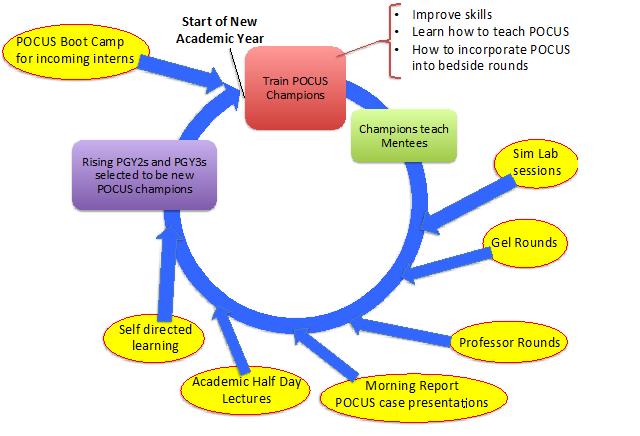
In the third phase, PCs are assigned four untrained residents, for whom they are responsible for supervising another 25 exams. By the end of the academic year, 100 Internal Medicine residents will have completed POCUS training. Rising PGY2s and PGY3s with the most interest and skill will then be selected as the new PCs for the following year. Champion training at the beginning of the second and following years will focus on skills for teaching, utilizing POCUS during bedside rounds and also in acute situations. All upper level residents will have basic POCUS training by this point, so the PCs now can focus on training the new interns. In the future the curriculum will expand to cover additional organ systems and POCUS education will be further augmented through additional means as shown in Figure 1.
Conclusions: POCUS is developing into an essential skill for Internal Medicine physicians practicing modern medicine, yet incorporating POCUS training into resident education is difficult when limited trained faculty exist. The “Teach the Teacher” model overcomes this obstacle by putting the responsibility of POCUS education into the stakeholders themselves. This model provides a platform for upper level residents to teach POCUS and allows interns the opportunity to learn while simultaneously taking care of their hospitalized patients. “Teach the Teacher” creates a self-perpetuating cycle that serves as the foundation for our curriculum. Furthermore, it produces a cultural shift towards embracing this technological skill within the field of Internal Medicine.