Background: Hospitalists on inpatient resident teaching services receive variable training in how to facilitate high-quality education during rounds. Teaching of cognitive skills such as clinical reasoning, acknowledging uncertainty, and non-cognitive behaviors such as eye contact are important techniques of effective educators. To enhance bedside teaching, the Hospital Medicine Division of the University of Michigan and Veterans Affairs Ann Arbor Healthcare System developed a novel program entitled Direct Observation of Clinical Teaching On Rounds (DOCTOR).
Purpose: Develop more effective inpatient-oriented clinical teachers.
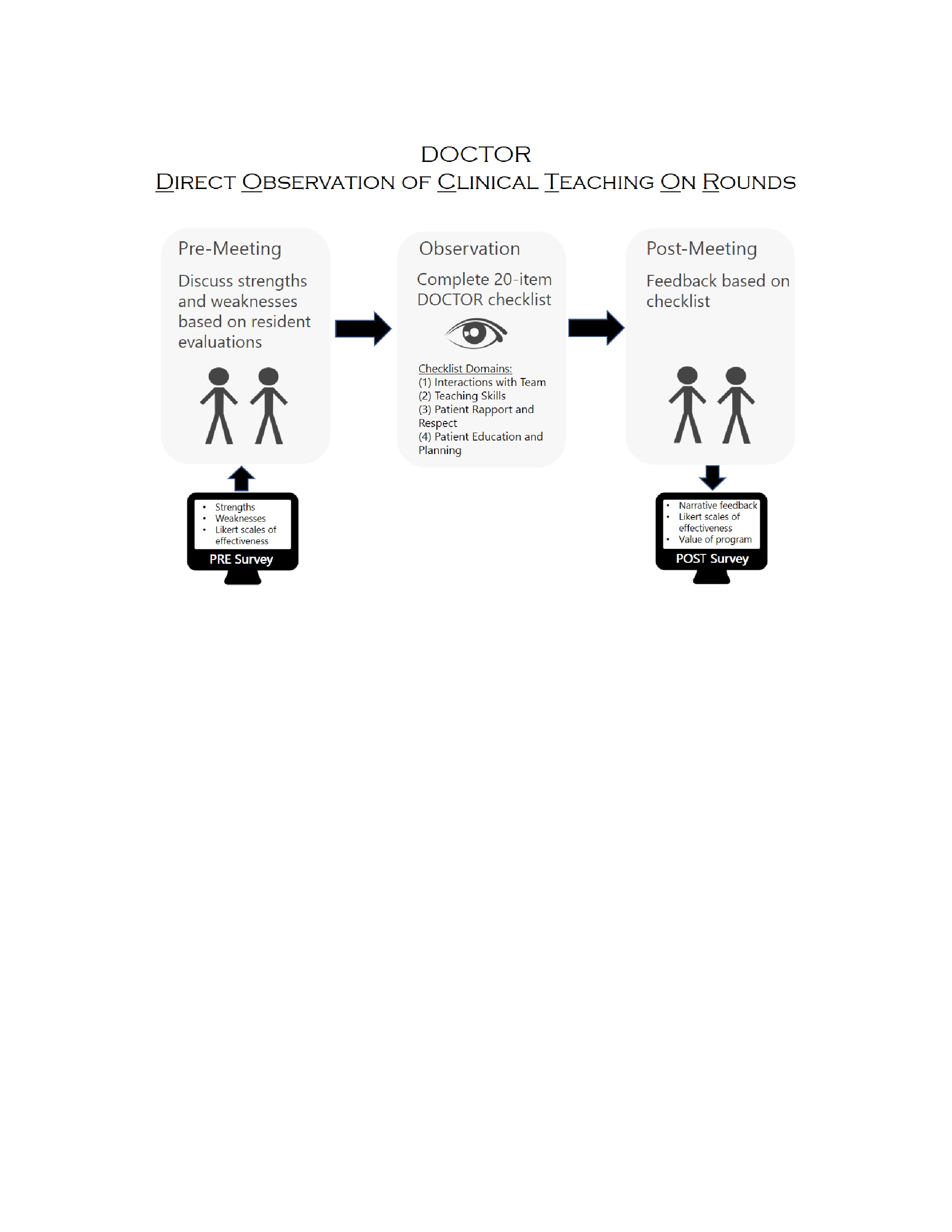
Description: Hospital medicine faculty rounding on a 2-week resident hospitalist service between 1 July and 30 September 2018 were included. Faculty members reviewed their teaching evaluations and completed a self-assessment rating of skills using a 5-point Likert scale (1=not at all effective, 5=highly effective) in the areas of teaching skills, interpersonal communication skills (ICS) with residents, ICS with patients, ICS with care team, time management, and overall. Next, faculty members were paired sequentially based on rounding schedule.
Each pair met to discuss self-assessments and observe each other on rounds. Observation included a 20-item checklist with four domains (Figure). The frequency of observed behaviors was recorded as: always/almost always, occasionally, rarely/never, or not applicable. The observer provided verbal feedback to the rounding faculty. Rounding faculty completed a Likert- based self-assessment and asked whether they would change their rounding practice as a result of the program. The observing faculty completed a survey on strengths and areas for improvement of the rounder.
Of the 12 eligible faculty members, 10 (83.3%) participated in the program, with six (60%) completing all assessments. Observers reported 76.7% of checklist items occurred almost always, 16.7% were observed occasionally and 6.7% were not applicable. Average self-rated effectiveness changed from pre-post in the following domains: ICS residents (3.9 to 4.3, p=0.20), ICS patients (4.1 to 4.3, p=0.60), time management (3.4 to 4.0, p=0.43), and overall (3.7 to 4.1, p=0.08). Effectiveness in teaching skills (3.6 to 3.6, p=1.0) and ICS care team (4.4 to 4.4, p=1.0) remained stable.
All nine observers who completed the post-observation survey agreed that it was a valuable experience. Eight (88.9%) indicated they would make at least one change in their rounding style.
Conclusions: Participation in the program was valuable to teaching hospitalists and led to improvement in overall performance. Continued expansion of the program to examine if resident evaluations of hospitalists improve after participation is underway.