Background:
Our study had the following objectives: (1) determine subintern's knowledge and attitudes toward members of the multidisciplinary team; (2) identify knowledge deficits in a subintern's ability to plan and execute inpatient discharges; (3) evaluate the impact of attendance at daily multidisciplinary rounds on subintern's knowledge and attitude toward members of the multidisciplinary team and the discharge process.
Methods:
Subinterns at our institution rotate at 4 different sites. Students have a similar level exposure to inpatient general internal medicine going into their subinternship. Only 1 of 4 sites conducts daily multidisciplinary rounds at which the senior resident from each medicine team presents the team's patients. Starting in October 2011, we instructed our subinterns to attend these rounds. From October 2011 to October 2012, we surveyed a total of 105 medicine subinterns across all 4 sites. The response rate was 67%. Students were surveyed both at the beginning and end of their rotation. We queried students on (1) their knowledge and perception of the role and relevance of members of the multidisciplinary team to care of hospitalized patients, (2) the utility of attending multidisciplinary rounds, and (3) the subintern's comfort level with discharge planning and execution. We compared student responses between sites with and without multidisciplinary rounds to determine the impact of these rounds on students' knowledge and attitude. All responses were recorded on a 1–5 scale, with 5 being the best possible score.
Results:
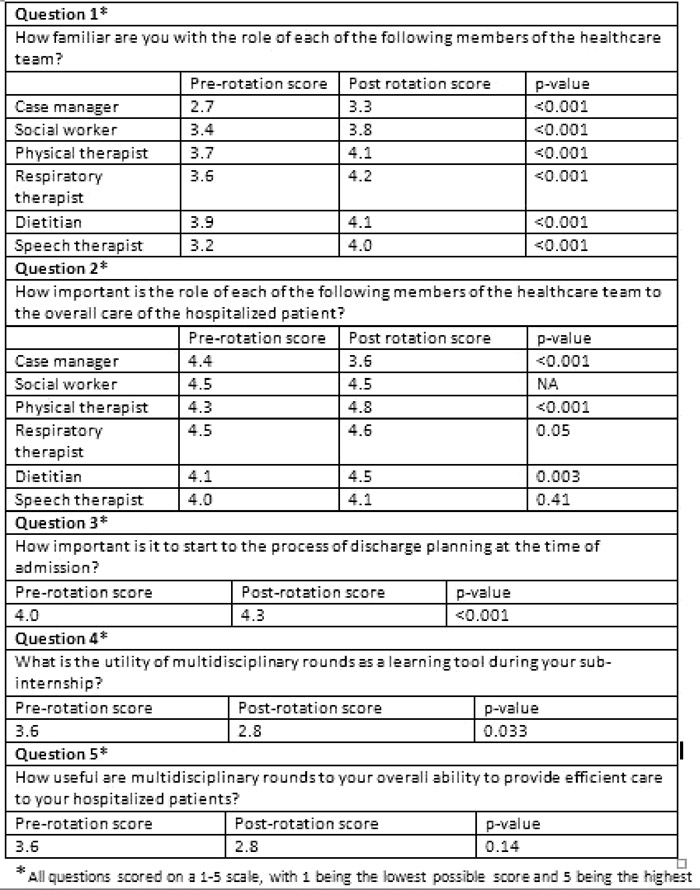
Over the course of the subinternship, there was a statistically significant improvement in students' familiarity with the role of members of the multidisciplinary team (Table). Students also got more comfortable in interacting with members of a multidisciplinary team (2.6–4.3, P < 0.001) and expressed greater appreciation of the importance of various members of the multidisciplinary team in providing comprehensive care to their patients (Table). There was marked improvement in students' reported ability to manage the discharge process, both in terms of determining discharge disposition (2.8–4.3, P < 0.001) and executing the discharge plan (2.8–4.1, P < 0.001). There was no difference in knowledge and attitude toward members of the multidisciplinary team or comfort with the discharge process between students who attended multidisciplinary rounds and students who did not. Students who attended multidisciplinary rounds reported a decline in perceived clinical and educational utility of these rounds by the end of the subinternship.
Conclusions:
Without any formal or specific curricular intervention, students' knowledge, attitude, and comfort level with roles of various members of the health care team and the discharge process showed reassuring growth throughout the 1‐month medicine subinternship. Attendance at multidisciplinary rounds did not improve students' experience with members of the multidisciplinary team or the discharge process.