Background: Hospital discharge is a complex process for patients, caregivers, and providers. A patients’ understanding of new diagnoses, medications, and appointments improves the capacity for self-care and post-discharge outcomes. A new “Team Discharge” initiative was piloted to improve patients’ understanding of the discharge plan through patient-centeredness and interdisciplinary communication during the critical transition from hospital to home.
Purpose: To improve patients’ understanding of the discharge plan.
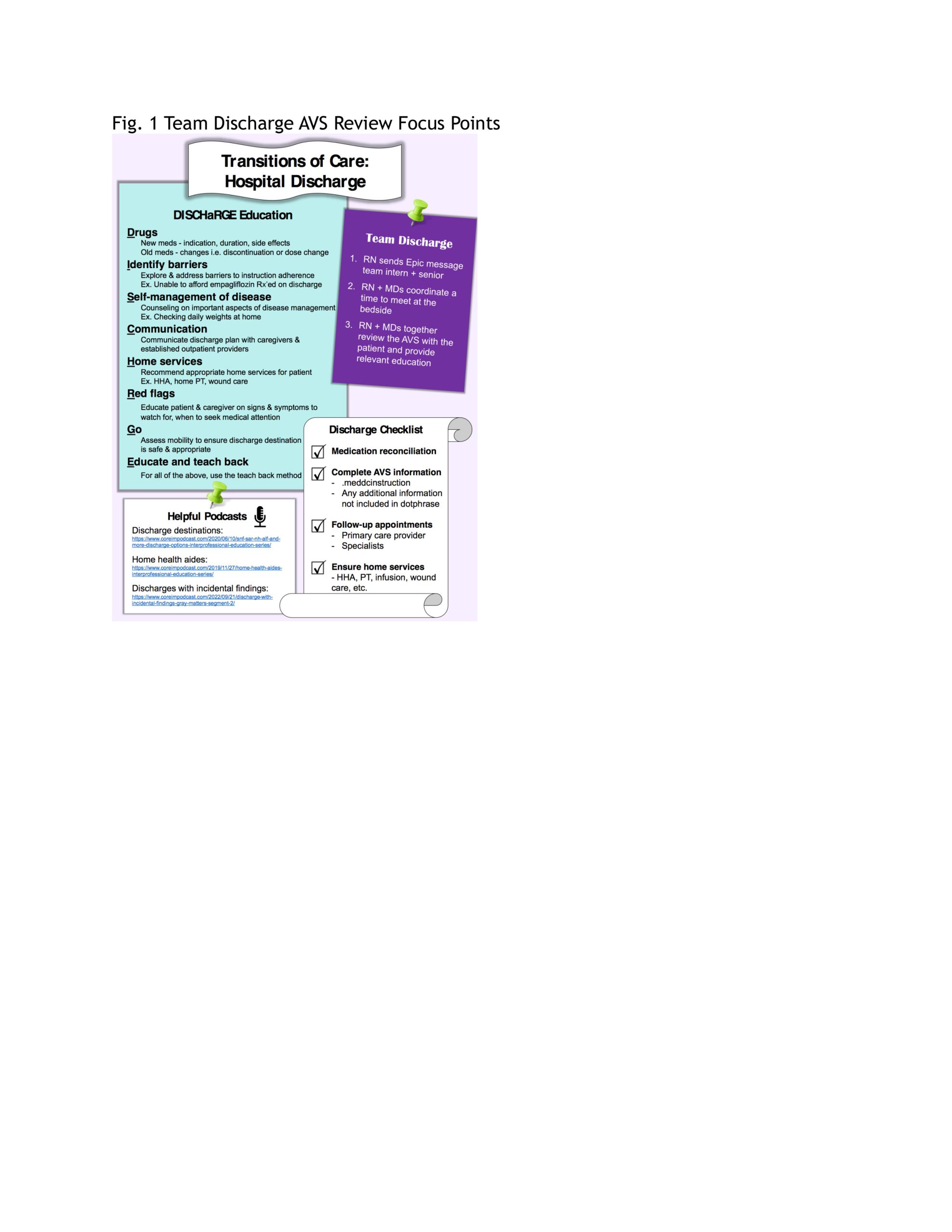
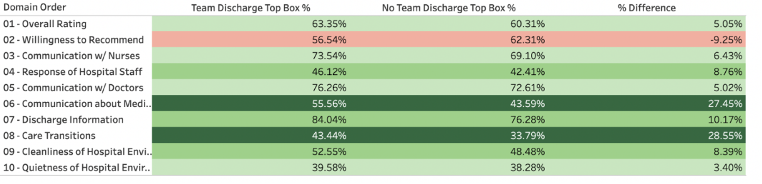
Description: We piloted the intervention on 5 medicine units from February 2022 through December 2022. The intervention included the following steps.First, the primary nurse messages the patient’s provider that the discharge paperwork is printed and all is ready to initiate Team Discharge. Next, the nurse and provider perform a thorough bedside review of all the discharge plans, medications including side effects, discharge instructions such as wound care or diet changes, follow-up appointments as well as the after-visit summary (AVS) as a team, as illustrated in Figure 1. Once the Team Discharge is complete, the primary nurse enters a smartphrase documenting the completion of the Team Discharge process in the patient’s chart. This ensures that every patient who had a team discharge is reportable. Using an EMR reporting tool, HCAHPS survey responses were linked to “Team Discharge completion” status, based on the presence or lack of a “Team Discharge” note during the encounter. Survey results from patients with a documented note of a completed Team Discharge were compared to patients without the intervention. Over 11 months, 5000 patients (50%) were documented as having completed a Team Discharge. Using HCAHPS surveys to measure the impact of the “Team Discharge” process, we noted an improvement in top box scores in many domains of patient experience. Notably, respondents who had a “Team Discharge” documented had a 26% increase in top box scores in the domain of Care Transitions (43% vs. 34%), 27% increase in the domain of Communications about Medications (56% vs. 44%) and 10% increase in the domain of Discharge Information (84% vs 76%), Figure 2.
Conclusions: The “Team Discharge” initiative provides an opportunity to bring the entire care team to the bedside at the time of discharge in order to help explain and clarify discharge instructions to patients in a collaborative manner. Compliance of the Team Discharge process continues to grow, and it is now the primary way patients are discharged from the hospital. While continued education and standardization can help maximize the benefits of this new way of discharging, initial data suggests improvement in several HCAHPS domains, especially Discharge Information, Care Transitions and Communication about Medications.