Background: In March of 2016, the CDC released guidelines recommending shorter duration of opioid prescriptions. While these guidelines have the potential to influence hospitalist practice, it is not clear whether discharge prescribing patterns have changed for hospitalized patients. We perform an interrupted time series analysis to examine changes in discharge opioid prescribing from an inpatient medical service at a single academic center.
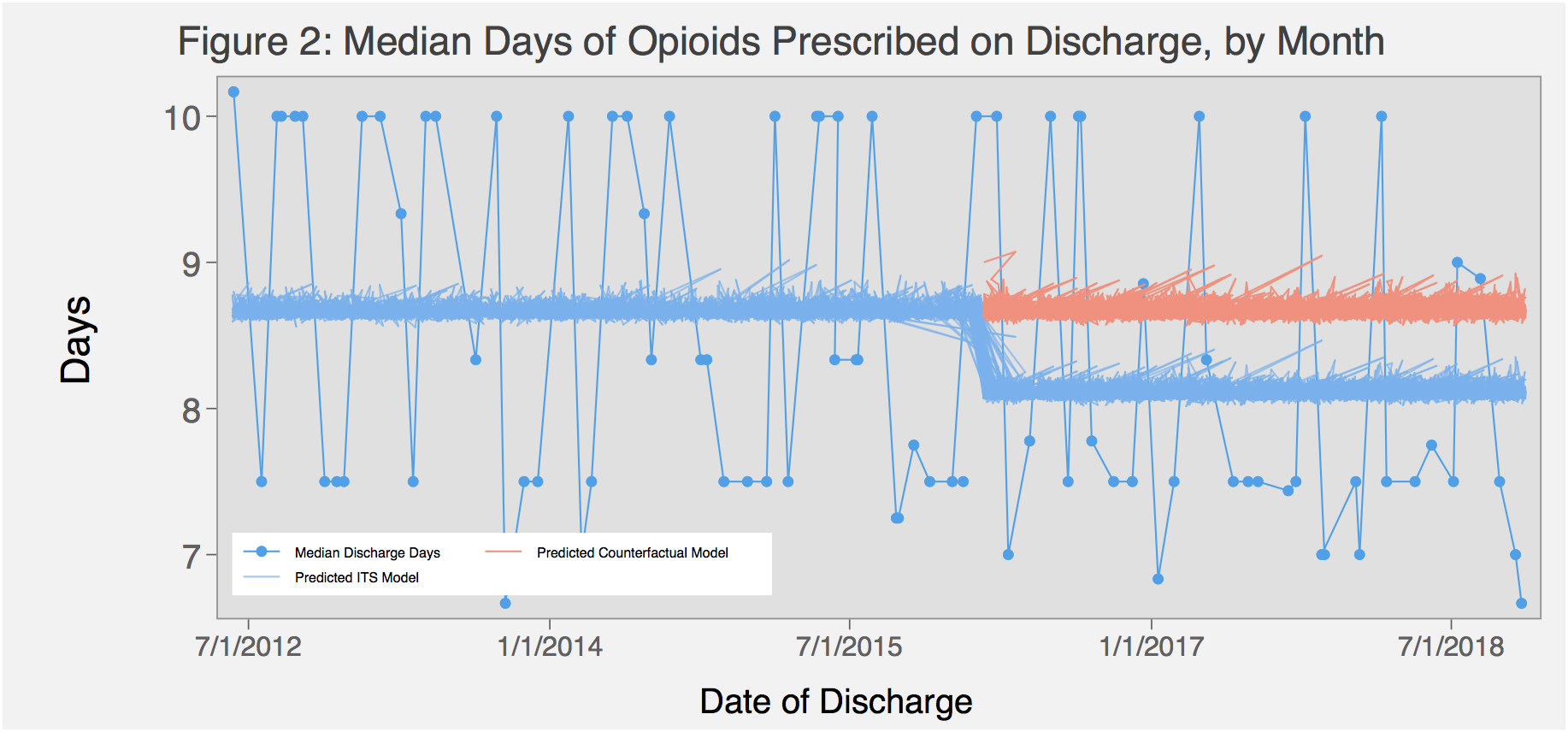
Methods: We used the electronic health record to identify all patients hospitalized on the acute care medical service at a 600-bed tertiary care hospital from 2012-2017, and stratified by whether they were on opioids at the time of admission according to provider medication reconciliation records. Patients were excluded if they had an ICD9 or 10 code for cancer-related pain or sickle cell disease, or who were on hospice or followed by the palliative care service. We calculated the number of opioid days supplied to the patient at discharge based on the discharge prescription signature and number of pills. All opioid prescriptions were standardized to morphine milligram equivalents (MMEs). We then calculated the median opioid days supplied at discharge by month, from 2012 to 2017. Multivariable Poisson regression analysis was used to assess for temporal trends in likelihood of opiate prescription and median days supplied, with an interrupted time series approach to test whether there was a significant change at the intervention point of March, 2016.
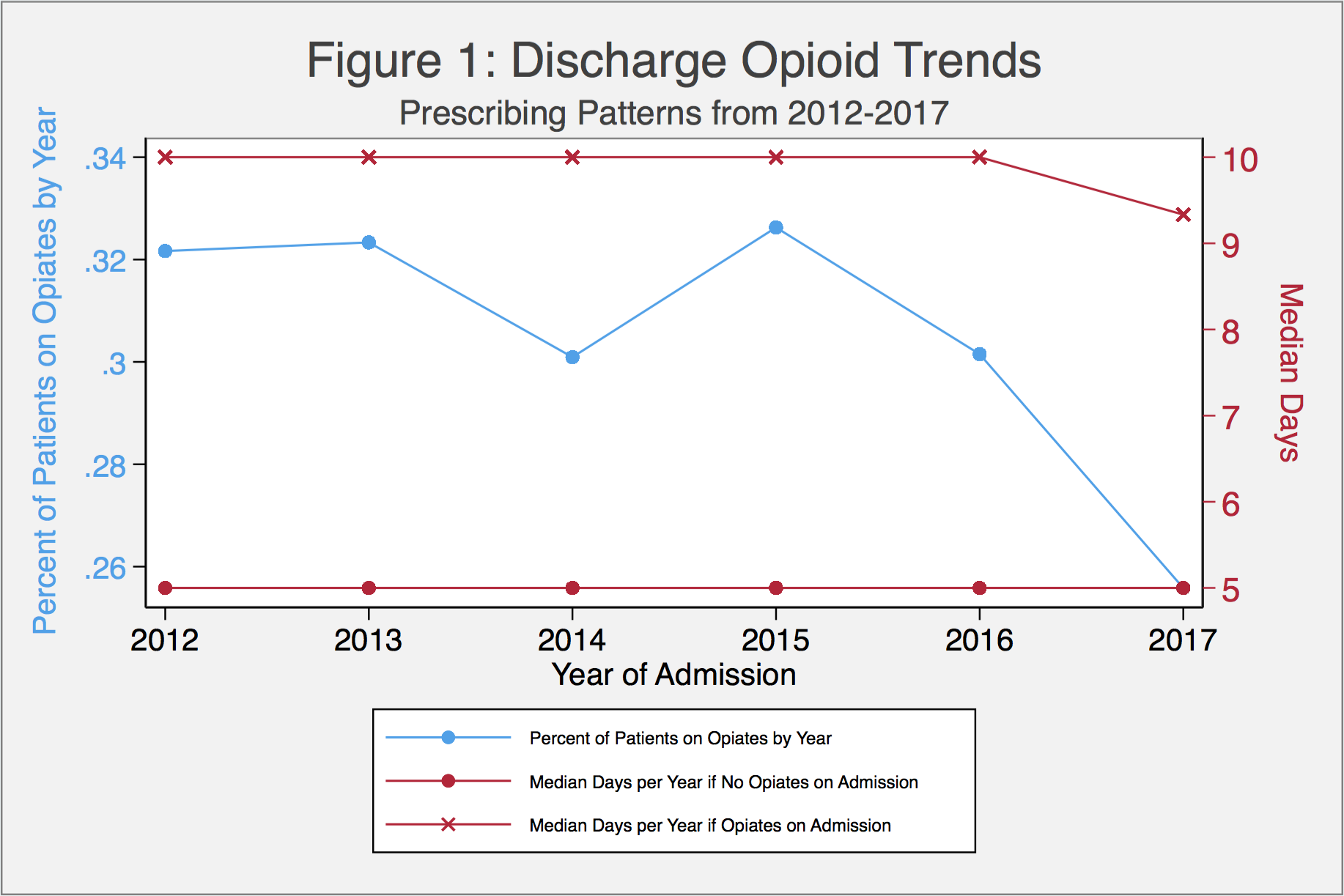
Results: We identified 19,759 medical inpatients who received opiates during their hospitalization, 23% of whom were not on opioids prior to admission. A total of 10,653 patients were discharged on opiates. The proportion of patients who were discharged with an opiate prescription declined over time (32.2% in 2012 to 25.6% in 2017, p<0.001; Figure 1). The median number of opiate days prescribed also declined over time, from 8.3 days in 2012 to 7.5 days in 2017 (p=0.02). The decline in median opioid days from 2016 to 2017 was statistically significant in patients taking opioids prior to admission (10 to 9.3 days, p=0.04). Though the median days prescribed on discharge in patients without baseline opiate use remained at 5 days from 2012 to 2017, there was a slight statistically significant decline in overall trend (p=0.02). After adjusting for patient level factors—age, sex, race, ethnicity, language, interpreter requirement, length of stay, ICU stay during admission, and van Walraven Comorbidity Index—we continued to find a significant decrease in opioid days supplied at discharge in all patients, with a significant decline post-March 2016 (rate ratio=0.93, p <0.001; Figure 2).
Conclusions: The percent of patients discharged on opioids from a hospital medicine service has declined over time, with a sharper drop from 2016 to 2017 than in years prior. The median number of days among those patients discharged on opioids has also declined over time. Patients on opioids at the time of admission are discharged with higher median days of opioids than those not previously on opioids – a trend that continued beyond the release of the 2016 CDC guidelines.