Background: Inpatient addiction consultant services are an innovative and proliferating tool used to confront the opioid epidemic. As healthcare systems seek to address gaps in care for patients with substance use disorder (SUD), the inpatient setting is increasingly understood as a unique opportunity for counseling, referral for treatment, and initiation of medication assistance treatment (MAT) for this vulnerable population. Substance use disorders, particularly opiate use disorder, have been linked to an increased rate of Against Medical Advice (AMA) discharges. AMA discharges are associated with increased mortality, readmission rates, and higher costs. Increasingly, clinicians are questioning the benefit of AMA discharges as a practice at all. The aim of our study was to evaluate the potential impact of a Hospital Medicine based opioid addiction consultation service on the volume of AMA discharges, particularly for those patients recommended to receive post-acute care.
Methods: The study was conducted at a Midwestern, urban, academic, tertiary referral center with a large Hospital Medicine group. All discharges from October 2018 through October 2019 were evaluated. Charts were reviewed by investigators for evidence of a SUD in the HPI, discharge summary, and progress notes. Charts were also reviewed for urine drug and serum alcohol testing. AMA discharges were categorized as “certainly” being related to opioid use disorder: when patient concerns for going into withdrawal were explicitly noted, “likely” related to opioid use disorder: when there was a clinical history of opioid use disorder and an inappropriately positive UDS but no explicit mention of withdrawal, or “possibly” related to opioid use disorder: when there was an inappropriately positive UDS but no clinical history of opioid use disorder. All AMA discharges were also screened for cocaine and alcohol use disorders. Recommendations for disposition to post-acute care facilities were captured based on physical therapy evaluations.
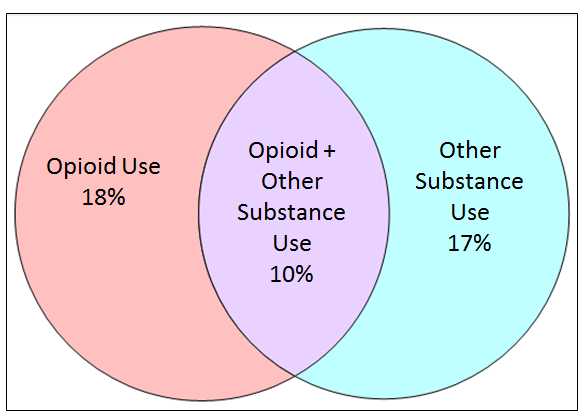
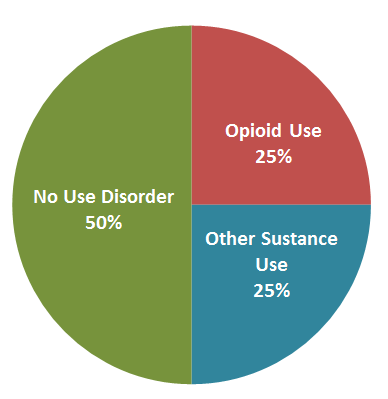
Results: A total of 6632 discharges were reviewed and 183 (2.8%) were identified as AMA. The average length of stay for an AMA inpatient encounter was 3.6 days, and 40 (22%) were observation encounters. Opioid use disorder was “certainly” or “likely” responsible for 35 (19%) of all AMA discharges. There was an additional 15 designated as “possibly,” for a total of 50 (27%) opioid related cases. Alcohol or cocaine use disorders were found in 49 (27%), of which 20 had concurrent opioid use (Figure 1). In total, 79 of the 183 (44%) AMA discharges were likely related to SUD. Post-acute care facility recommendations were made for 16 (8.7%) patients prior to AMA discharge. Of those with post-acute care recommendations, 8 had substance use disorders with opioid use disorder being associated with 4, representing 2% of all AMA discharges (Figure 2).
Conclusions: AMA discharges were uncommon in the Hospital Medicine group evaluated in the study. Of the AMA discharges, nearly half were for patients with known or suspected substance use disorders. The implementation of an opioid addiction consultation service would likely significantly decrease the volume of AMA discharges, which are harmful to patients and healthcare systems alike, but have only a marginal impact on ensuring patients reach a post-acute facility. We hope that focusing on the contribution of SUD to AMA discharges continues to galvanize the hospital medicine community to develop specific inpatient tools to confront this crisis.