Background: Inter-hospital transfer (IHT, the transfer of patients between hospitals) exposes patients to risks of discontinuity of care, including errors in communication. However, the association between communication among providers during IHT and patient outcomes has yet to be rigorously studied due to limitations of administrative data to adequately capture quality of communication. In this study, we used medical record review to evaluate the association between provider communication during IHT and clinical outcomes.
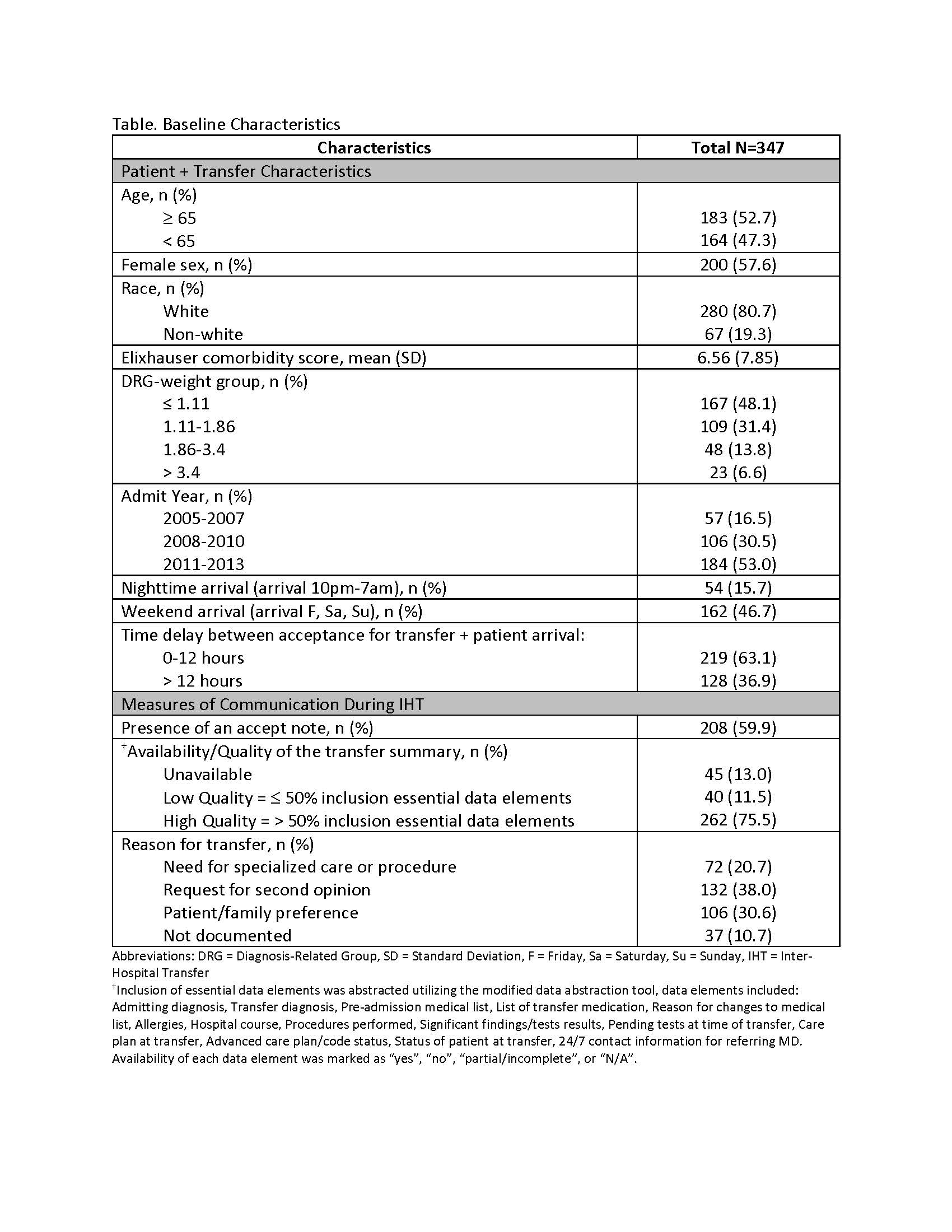
Methods: We performed a retrospective analysis of 347 randomly selected patients from a previously gathered cohort of patients ≥ age 18 transferred to the general medical service of a 793-bed tertiary care hospital from another acute care hospital between January, 2005 and September, 2013. Select measures of communication during IHT were abstracted via targeted medical record review using a modified version of a previously validated abstraction tool, and included: (1) Presence of a patient accept note, i.e., a summary of clinical information documented by the accepting clinician at time of patient acceptance for transfer; (2) Availability/quality of a transfer summary as documented by the transferring clinician at time of transfer, categorized into unavailable, low quality and high quality, based on percent inclusion of essential data elements; and (3) Documented reason for transfer, categorized into need for specialized care/procedure, second opinion, patient/family preference, or not documented. Data was abstracted by one of four trained clinicians, with monthly meetings to review cases to ensure consistent techniques. Outcome measures were collected administratively and included transfer to the ICU within 48-hours of patient arrival and in-hospital mortality. Covariates for adjustment (also from administrative data) included patient demographics, comorbidity, illness severity, admit year, and timing of arrival. We used descriptive statistics to determine baseline characteristics and performed multivariate logistic regression to obtain the adjusted effect of measures of communication on the composite clinical outcome of ICU transfer or in-hospital mortality. Secondary analyses evaluated each outcome independently.
Results: Patient and transfer characteristics and baseline measures of communication during IHT are shown (Table). In adjusted analyses, we found that presence of an accept note was associated with lower adjusted odds of ICU transfer/in-hospital mortality (aOR 0.21; 95% CI 0.07-0.61), largely driven by lower adjusted odds of ICU transfer. Availability/quality of a transfer summary and reason for transfer were not significantly associated with the composite outcome or either individually.
Conclusions: In this evaluation of IHT patients to general medical services, we found that the majority of IHT patients had a documented accept note, arrived with a high-quality transfer summary, and had documented reasons for transfer that were fairly equally distributed between measured categories. We also found that the presence of an accept note is associated with lower rates of ICU transfer after adjusting for other patient and transfer factors, suggesting that improved intra-hospital communication during IHT may impact patient outcomes.