Background: Despite a public health crisis – over 500,000 individuals have died from opioid overdoses since 2000 – and the availability of effective therapies, most patients with Opioid Use Disorder (OUD) are not offered treatment. Medication-Assisted Treatment (MAT), such as with buprenorphine, is associated with significantly higher rates of abstinence and follow-up, lower rates of readmissions and criminal activity post-discharge, and improved mortality. Patients with OUD may be hospitalized for several days or weeks at a time, frequently for complications directly related to their substance use disorder, and may be at various stages of dependency during their admission. Thus, the hospital setting provides a unique opportunity to deliver education and offer patients treatment with buprenorphine. Few hospital-based programs exist nationwide that offer buprenorphine induction on medical or surgical wards, and these programs are typically supported by physicians with addiction medicine specialty training. The scope of the opioid epidemic makes this a non-scalable model, thus hospitalists should also be able to provide this service.
Purpose: We created a hospital-based medicine-led interprofessional service (“The B-Team” (Buprenorphine)) that screens patients for buprenorphine induction, assists in starting treatment, facilitates linkage with an outpatient maintenance clinic, and provides institutional education in an effort to reduce stigma associated with OUD.
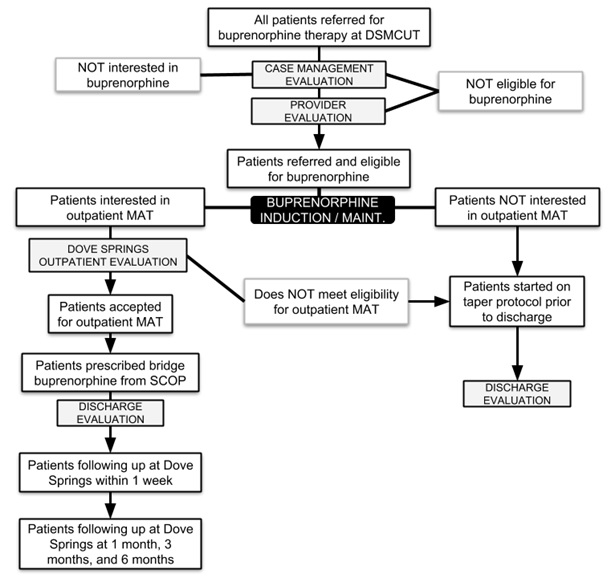
Description: We conducted a literature review to understand the current landscape of hospital-based MAT programs. We then developed an inpatient buprenorphine induction protocol specifically for our institution (Figure 1) and created reference guides for providers, nurses, and pharmacists. We strengthened relationships with outpatient MAT clinics to provide warm-handoff linkages for patients upon discharge from the hospital. The program was launched in mid-September 2018. Patients are referred to the “B-team” by the primary hospital team. A social worker then screens the patient for his or her readiness for change. If qualified, a clinical provider initiates therapy in concert with the primary team and ensures linkage with the outpatient clinic at discharge including prescribing bridge maintenance therapy until the outpatient appointment. Within the first 8 weeks, 30 consultations were performed in our 211-bed hospital. We provided stigma reduction efforts in all cases. Ten patients were ultimately linked to outpatient therapy. At three months after program launch, seven of these patients continue to be engaged in therapy.
Conclusions: A robust interdisciplinary consultation program could be an effective model for providing hospital medicine-based therapy for inpatients with OUD. Opportunities to grow the program include expanding services to the emergency department and eventually training primary teams to initiate buprenorphine therapy.