Background: Hospital-acquired delirium is serious, leading to increased falls, pressure ulcers, length of stay, cost, patient institutionalization, and patient and caregiver distress. In addition, it is associated with mortality rates as high as 35-40% within one year in older patients who develop delirium. Programs targeted at delirium prevention and treatment may affect these outcomes. We aimed to determine if a structured delirium care pathway is associated with improved clinical outcomes in hospitalized adults on a medicine service in a large, urban academic medical center.
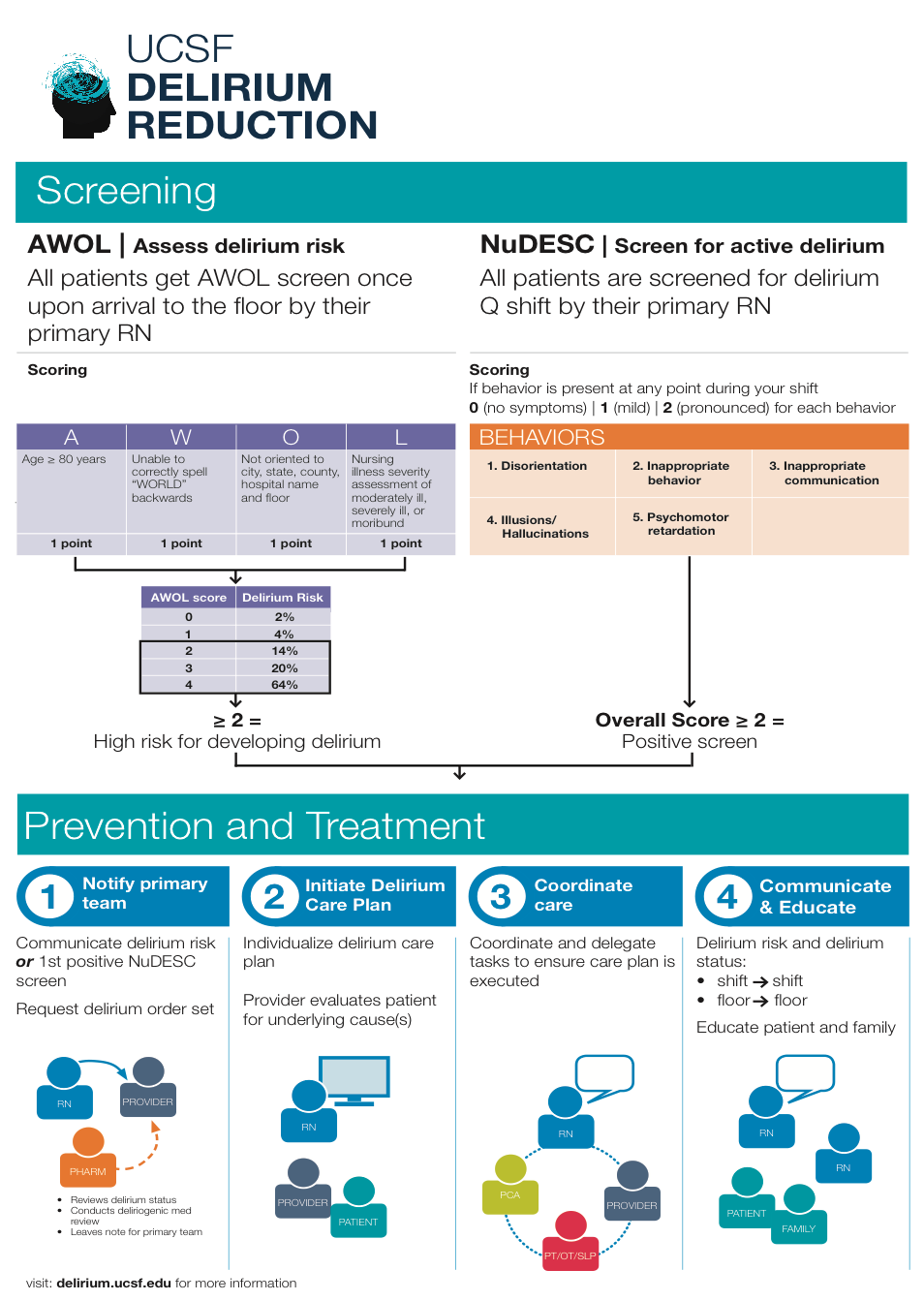
Methods: In this retrospective cohort study, we compared outcomes before and after a comprehensive, multi-disciplinary delirium care pathway was implemented on three medicine units (one step down unit, two acute care units). The pathway included delirium risk assessment upon admission, delirium screening by nurses every twelve hours, and a targeted non-pharmacologic care bundle implemented through a delirium order set for high risk and delirious patients [Figure 1]. We included all patients >= 50 years old hospitalized for at least 24 hours on three general medicine units from 1/9/2016–1/8/2017 (pre-pathway) and 1/9/2017-1/8/2018 (post-pathway). Patients who spent any time in the intensive care unit were excluded. Primary outcome was length of stay. Secondary outcomes included restraint use, safety attendant use, hospitalization cost and 30-day readmission. Since delirium screening was only implemented with the care pathway, delirium rates could only be measured in the post-pathway period. Outcomes were compared between time periods using multivariable generalized linear, Poisson and logistic models as appropriate, adjusting for clinical variables that were significantly different between groups.
Results: 5419 patients were included (2594 patients pre-pathway, 2825 patients post-pathway). Average age was 70±13 years; age and other demographic variables did not change over time. Mean length of stay decreased after the intervention by 0.8 days (95% CI 0.8, 1.1; p<0.0001). Hospitalization direct cost decreased by an average of $850 per patient (95% CI -1505, -197; p<0.0001) and odds of readmission were reduced by 30% (OR 0.7, 95% CI 0.6, 0.7; p<0.0001). Patient safety attendant (p=0.3) and restraint (p=0.2) use did not change. The rate of delirium did not significantly change in the post-pathway period (p=0.2), but there was a trend towards improvement with a reduction from a peak of 178 delirium days per 1000 patient days down to 129 delirium days per 1000 patient days.
Conclusions: Implementation of a comprehensive, multi-disciplinary delirium care pathway on three general medicine units was associated with reductions in hospital length of stay, hospitalization cost and 30-day readmissions. Further study is needed to understand any impact on patient experience and mortality outcomes.