Background: Clinical documentation integrity (CDI), a process by which documentation is optimized to be both congruent with Centers for Medicare and Medicaid (CMS) terminology and reflect patient severity of illness, is widely used in healthcare to ensure appropriate coding for hospital reimbursement and improve accuracy of research and quality outcomes. CDI optimization is often performed by clinical documentation specialists, who send CDI queries to providers to modify incongruent terminology. However, this administrative burden incurs additional costs and time, and CDI queries add to documentation burden which can contribute to physician burnout.
Purpose: We created a custom spell-check dictionary in Epic to help clinicians identify words that triggered CDI queries with the intention of reducing documentation burden and query volume.
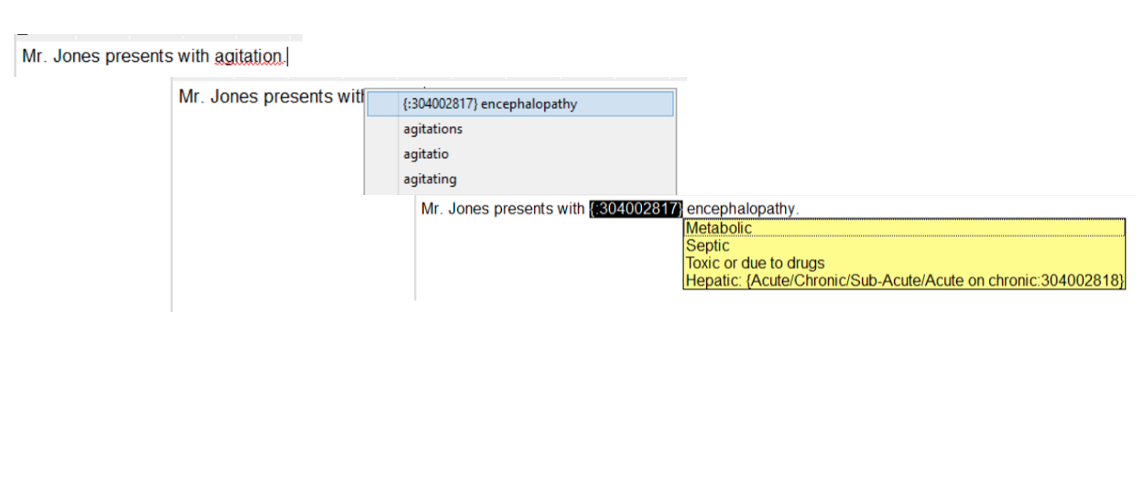
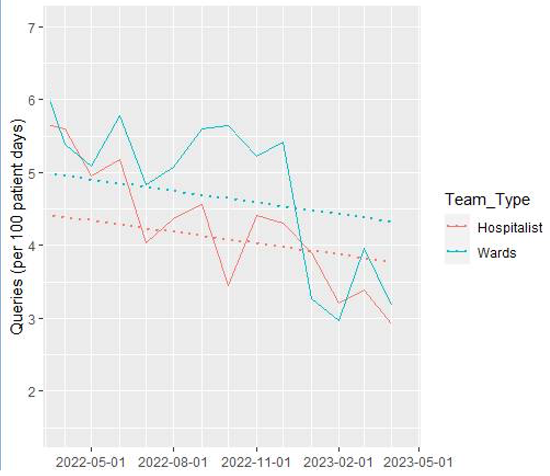
Description: At our institution, clinical documentation specialists manually review and identify incongruent terminology in patient notes and send CDI queries to clinicians to modify their documentation when appropriate. In our hospital medicine division, CDI queries have been identified as a physician dissatisfier, and in a survey of hospitalists, 40% (n=14) reported being unsatisfied with the current CDI query process, with nearly 55% (n=19) reporting that it negatively impacted their clinical experience. To address this, we leveraged the existing spell check feature in Epic to create a custom, shareable dictionary (“CDI-dictionary”) in Epic that recognizes words which are commonly used in patient notes but are incongruent with CMS terminology. The CDI-dictionary will either autocorrect those words or mark them as misspelled, and suggest documentation-compliant alternatives in real time. For example, “agitation” is a commonly used term but lacks the diagnostic specificity to be recognized by CMS. It would be recognized as misspelled, and when the user clicks on this word, the CDI-dictionary will recommend replacing it with another CMS-recognized form of encephalopathy instead, such as “toxic-metabolic encephalopathy” (Figure 1).The CDI-dictionary was rolled out to all clinicians in our Division of Hospital Medicine in November 2022, accompanied by a demonstration and monthly reminders. After six months, hospitalists were surveyed about their experiences. Of 27 respondents, 59% (n=16) reported making changes to their notes based upon recommendations from the CDI-dictionary. Of the 13 hospitalist who responded about usability, 85% (n=11) found the CDI-dictionary easy to use. When evaluating volume of CDI queries sent per month, there was a decrease beginning December 2022. In the six months prior to the release of the CDI dictionary (July – December 2022), there were 1711 queries sent (285/month). In the six months following the release (January – June 2023), there were 1466 queries sent (244/month), with reductions specifically for terminology from the CDI-dictionary. Overall, there was a 14% drop.
Conclusions: We developed a custom EHR spell-check dictionary to identify words that would commonly trigger CDI-queries and allow for real-time modifications with suggested, CDI-compliant terminology. Initial data suggest that our CDI-dictionary was easy to use and influenced clinician behavior, ultimately reducing the total number of queries sent. This reduction in queries could impact administrative burden and clinician dissatisfaction.