Background: Migraine headache (MHA) is a common pediatric disorder, which frequently leads to hospital admission. Inpatient MHA treatment involves various medications, including a combination of fluids, antiemetics, non-steroidal anti-inflammatory drugs, steroids, and anti-convulsants. Severe or recalcitrant headache may require more aggressive therapies, including dihydroergotamine (DHE). Opiates are not recommended in the treatment of MHA; however use is still seen. Adult literature shows that more than 58% of MHA patients have a psychiatric comorbidity (PC); these patients present unique challenges in the treatment process and often fail standard therapeutic interventions. Little is known about the influence of PC on the effectiveness of MHA treatment in pediatrics. The objective of this study was to determine national trends in the treatment of MHA in pediatric patients and the influence of PC on treatment effectiveness as measured by medication use, length of stay (LOS) and readmission rates.
Methods: We performed a retrospective cohort study of patients admitted to 51 tertiary care children’s hospitals using Pediatric Health Information System (PHIS) database. We included patients, aged 1-18, with ICD 9 and 10 codes for migraine as the principal diagnosis, hospitalized between 1/1/2010 and 6/30/2018. Psychiatric comorbidity was identified by presence of ICD 9 and 10 codes. Baseline demographics, medications and outcomes were compared between patients with and without PC using the Fisher exact or Wilcoxon-rank sum tests, as appropriate for the data distribution.
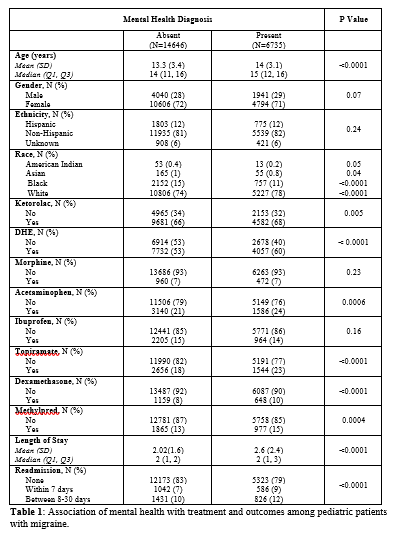
Results: Of the total 21,381 patients in the study, 6735 (31%) had underlying PC. Significant differences were noted in demographics between the two groups( Table 1), with the group with PC noted to be older. Variation was also noted by race. Patients with PC were significantly more likely to receive most anti-migraine medications, except for use of opiates and ibuprofen. Opiate use was noted in 7% of all cases. Patients with PC also had a longer mean LOS (p<0.0001) and higher readmissions(p<0.0001).
Conclusions: For patients admitted for treatment of MHA, the presence of PC leads to increased hospital use and a secondary burden on national health care resources. In addition, PC is associated with an increased use of most medications. Speculation as to the cause of the PC effect on MHA treatment includes a shared dysfunction of the serotonergic system in both diagnoses and overuse of medications derived from impaired coping behaviors. Alternative means of pain management may need to be considered for improved efficacy of treatment for MHA in these patients. Studies in the adult literature have shown that a combination of pharmacological and behavioral therapy is necessary for effective treatment of MHA in patients with PC. Further studies in pediatrics is needed to develop advanced pathways directing management of MHA in this special population.
.