Background: Health information technology (HIT) has the potential to decrease rates of hospital-acquired conditions. The Patient Safety Learning Lab (PSLL) developed a suite of HIT tools to engage patients, families, and providers in identifying, assessing, and reducing patient safety threats. The goal of this current evaluation is to quantify the effects of this intervention on safety-related processes of care.
Methods: The PSLL suite of tools included 1. Patient SatisfActive, where nurses solicited, documented, and shared patient/family needs, concerns, and expectations; 2. Patient Portal, a patient-facing application with personalized information on safety, the care team, medications and test results; 3. Fall TIPS, a program where nurses completed a personalized falls prevention plan for each patient; 4. Bedside Display, a computer screen-saver to help care team members be aware of patient-specific care and safety measures; and 5. Patient Safety Dashboard, which consolidated and displayed real-time electronic health record (EHR) data for 13 safety domains. These tools were implemented in a stepped-wedge trial in which units switched from usual care to the intervention in six “steps” at randomly selected points in time on 12 units in neurology, oncology, and medicine services between December 2016 and May 2018. To measure the effects of the intervention, process measures associated with the 13 safety domains were derived from EHR data. Results were analyzed using multivariable Poisson regression, using a random effects model by patient and by unit, and adjusted for study month (i.e., temporal trends) and clinical service. The primary predictor was before vs. after each unit switched from usual care to the intervention.
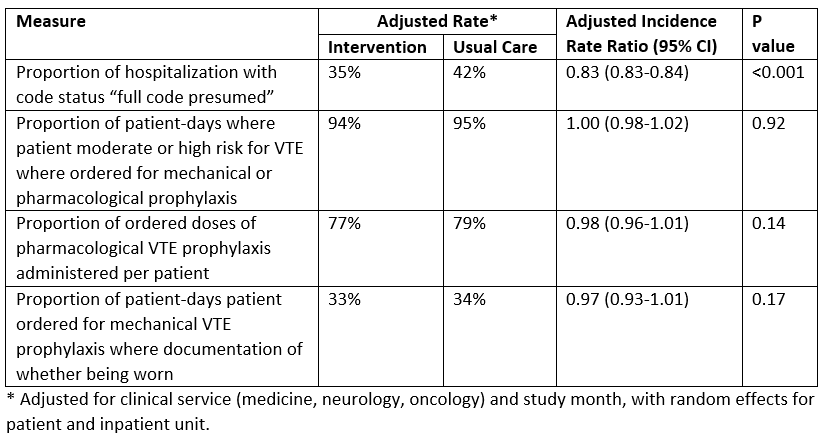
Results: There were 18,660 patient admissions in the study, with 12,805 (69%) in the intervention arm. Results to date are available for code status documentation and VTE prophylaxis. Adjusted for temporal trends, the intervention was associated with a significant 17% relative decrease in “full code presumed” status (i.e., failure to have a code status discussion). There was no association between the intervention and any of the 3 VTE prophylaxis measures (Table).
Conclusions: The implementation of a suite of HIT tools shows inconsistent effects to date, with a positive effect on code status documentation and none for VTE prophylaxis. Reasons for this may be related to the simplicity of the decision support (e.g. it is clear what a “red flag” for code status means, while a red flag for VTE prophylaxis could mean one of several deficiencies in care). Further analysis of the remaining process measures will provide a fuller picture of the effects of this intervention, with implications for how best to design and implement these types of HIT tools to improve inpatient safety.