Background: Code status specifies the action healthcare providers should take in the event of cardiac arrest. However, multiple studies have shown that patients with do-not-resuscitate/do-not-intubate (DNR/DNI) orders have worse outcomes and do not consistently receive standard of care when controlled for other variables. Several studies have demonstrated that physicians behave differently towards patients with DNR/DNI orders, but little research exists looking into whether DNR/DNI status affects the practice of other members of the care team. To our knowledge, no study has surveyed nurses regarding care delivery for patients based on code status.
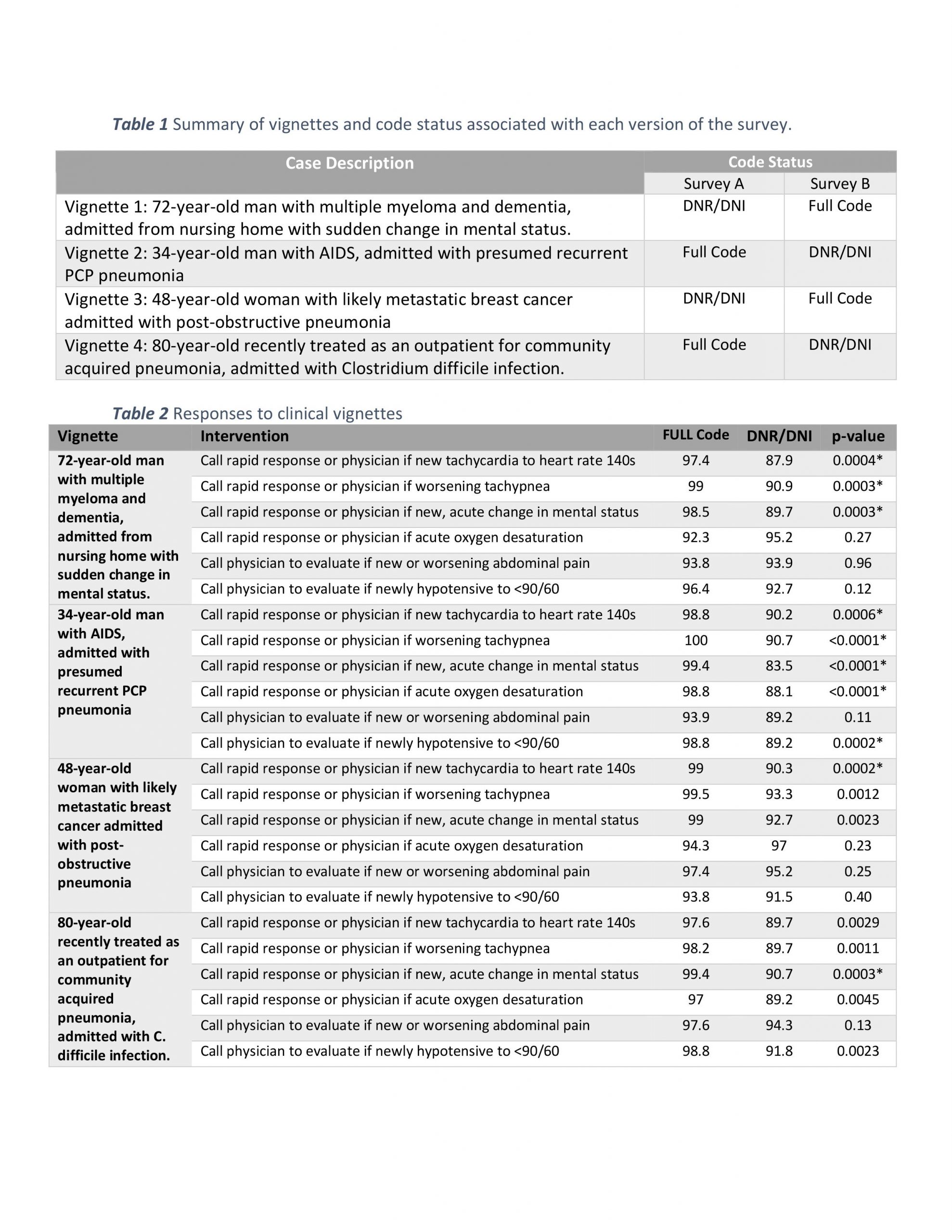
Methods: We conducted a randomized survey of nurses at two local hospitals to assess whether a patient’s code status affected nurses’ medical decision making. We created two versions of a survey that contained four previously published clinical vignettes followed by a series of questions regarding specific interventions for the patient that were tailored to reflect nursing escalation of care. The surveys differed only in the code status (Full Code vs. DNR/DNI) assigned to each vignette.
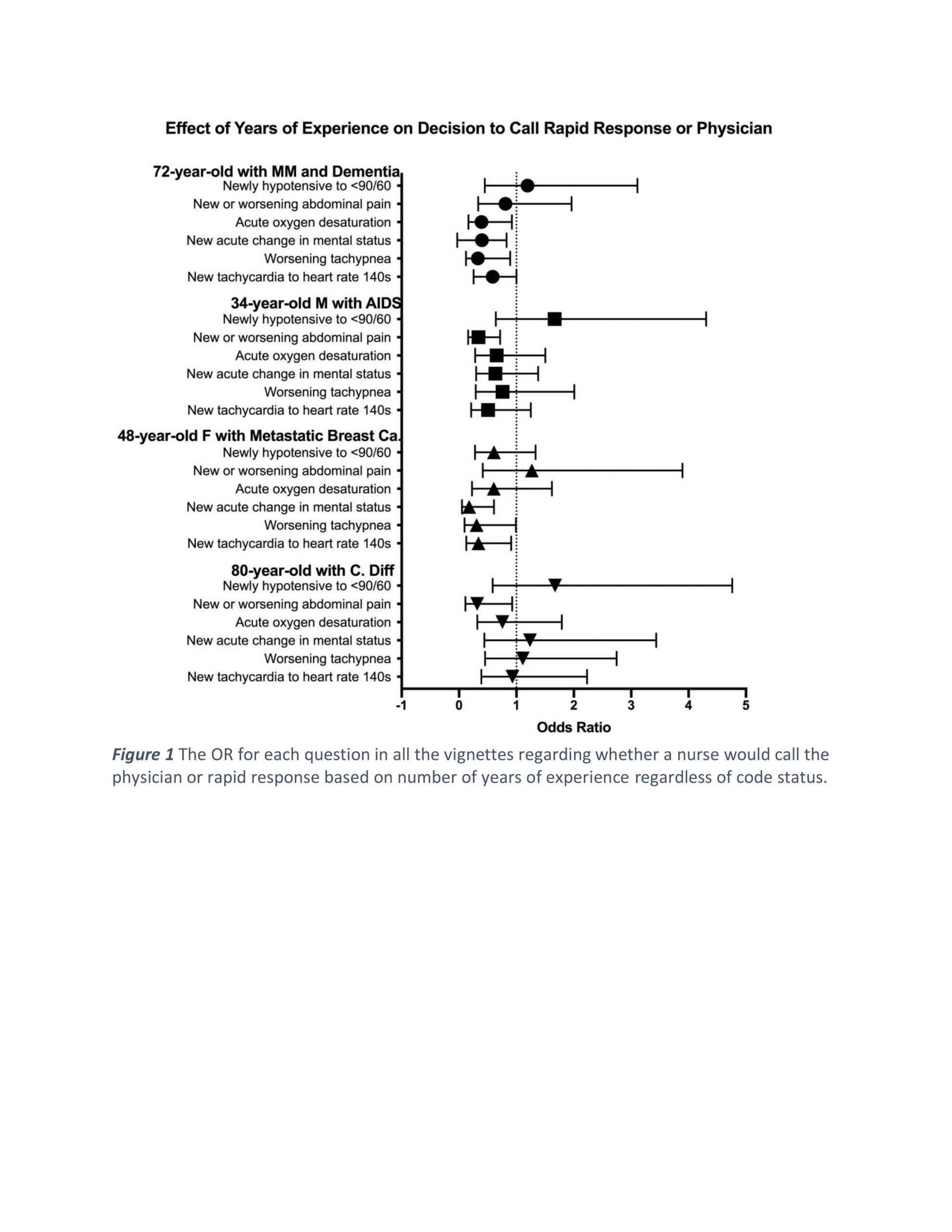
Results: A total of 358 nurses responded to the survey. For all four vignettes, respondents were less likely to say they would call rapid response or a physician for patients with a DNR/DNI status who developed tachycardia (p-values <0.001). Tachypnea and changes in mental status were also less likely to have nurses escalate care for patients with DNR/DNI status. Nurses were equally likely to call the physician for development of abdominal pain or new hypotension (p-values > 0.05). Nurses with greater than three years of experience were overall less likely to escalate care throughout the four vignettes and various questions for each (OR < 1).
Conclusions: This multi-center study is the first to demonstrate that code status affects nurse clinical decision making, and it joins a growing body of research that demonstrates the limitations code status designations create with regards to patient care. The presence of a DNR/DNI order may affect nurse’s willingness to alert other members of the care team to changes in clinical status unrelated to cardiopulmonary resuscitation. The insight into number of years of experience for nurses also helps identify where interventions can best be applied to help improve care delivery for patients with DNR/DNI orders. By acknowledging and addressing that patients with DNR/DNI orders receive different care, we can work to create a system where patients are treated equally regardless of their choice of code status.