Background: Diabetes is common, present in up to one third of hospitalized patients and up to 50% of critically ill patients. Studies have shown that hyperglycemia among hospitalized patients leads to worse clinical outcomes and increases readmission rates by over 30% relative to normo-glycemic patients. Insulin is the only medication recommended for treatment of diabetes in the hospital. Basal bolus therapy is the evidence-based approach. Despite the prevalence and impact of these conditions, and even though there are clinical practice guidelines, attention to optimal treatment can get lost in the shuffle of competing medical issues, complex physiology and the chaos of the acute care environment.
Purpose: To develop and trial a tool within the electronic health record (EHR) that performs real-time blood glucose and insulin order evaluation of all inpatients, and then provides evidence-based treatment recommendations to the inpatient care team thereby improving glycemic control, and potentially, clinical outcomes.
Description: An andon is a way of notifying a worker of real-time operational conditions. A glycemic andon is one that displays alerts within the EHR about a patient’s current glycemic status (outcome metric) as well as insulin order status (process metric). If a patient’s blood glucose value is at goal, a green andon will be displayed for that patient. When blood glucose is outside the goal range, and the insulin regimen is consistent with our evidence based approach, a yellow andon is displayed. However, if the blood glucose is outside of range and the insulin regimen needs to be adjusted, a red andon is displayed with instructions indicating what type of insulin to add. The signal is updated for every patient every sixty seconds. In addition to the display of the andon within the individual patient’s chart, the andons for all patients are displayed on a large wall mounted monitor in their respective units. This wall mounted monitor is known as the Clinical Andon Board (CAB) and it creates real-time situational awareness of glycemic control for the entire care team as well as patients, families and visitors.
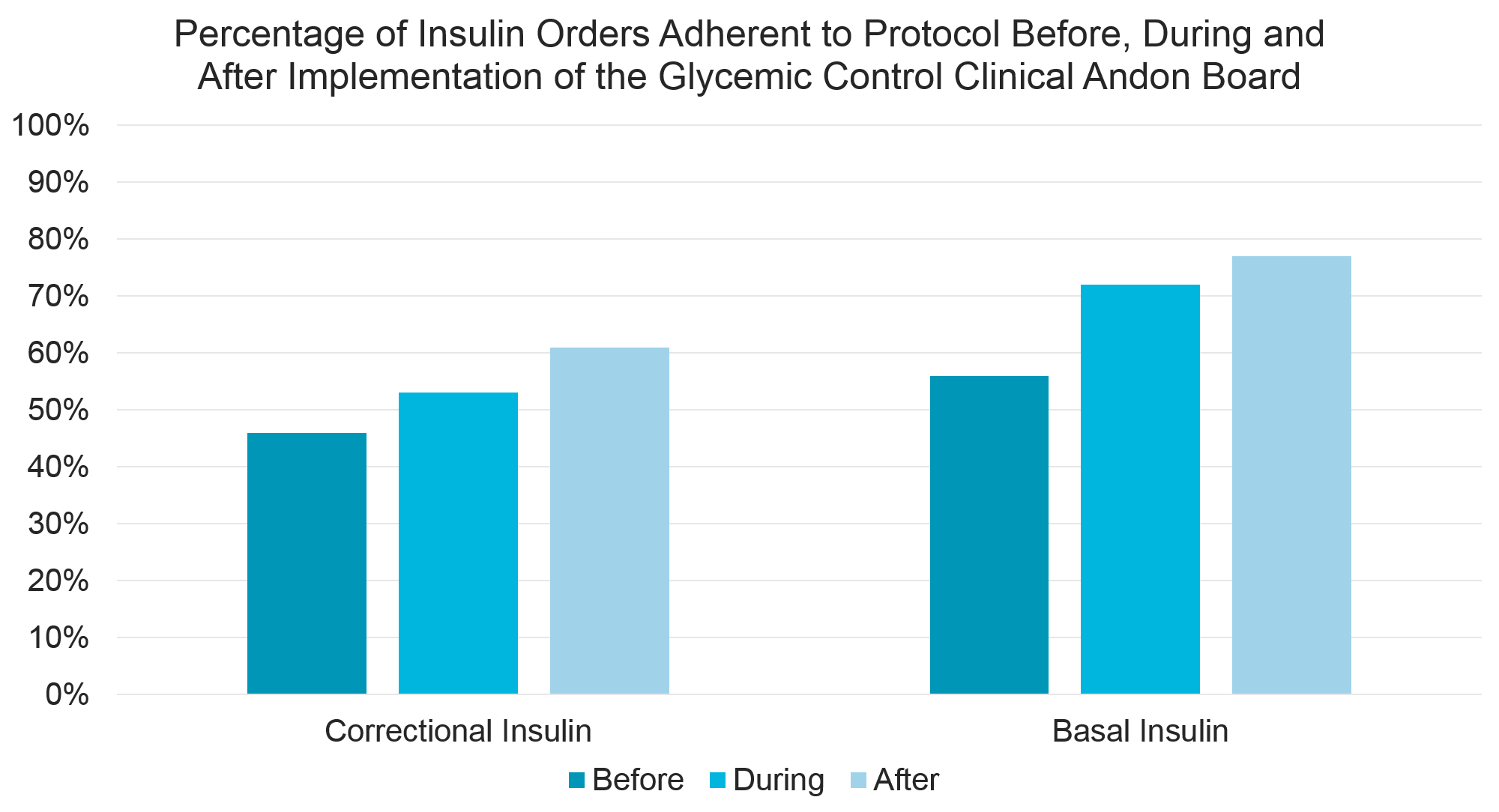
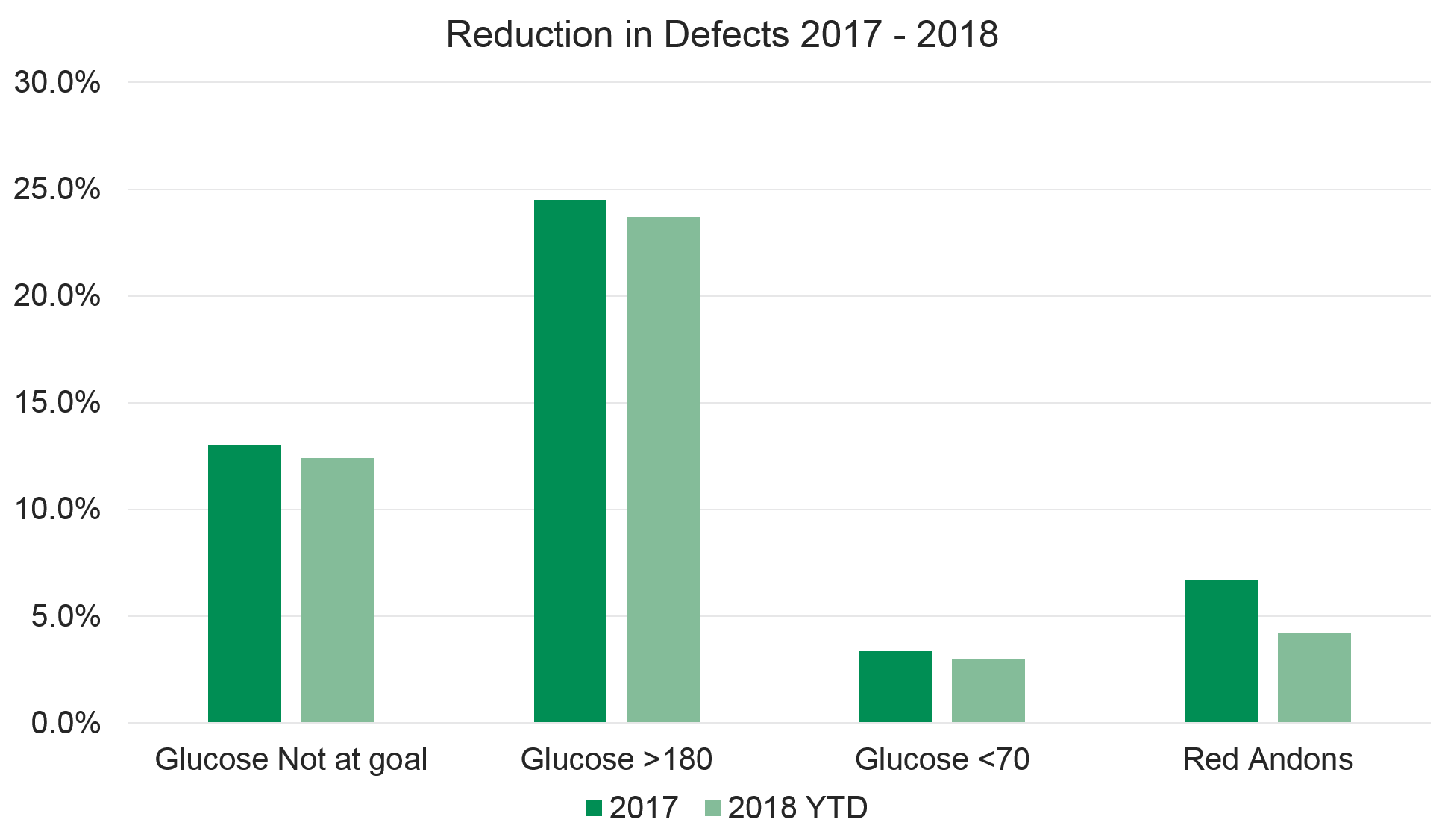
Conclusions: The CAB is an effective and efficient way to create real-time situational awareness of poor blood glucose control, and to provide clinical decision support within provider work flow to improve glycemic control. In addition to increasing evidence based prescribing practices and better glycemic control, the CAB improves provider knowledge of optimal blood glucose management strategies and has been useful in evaluating our standardized order sets.