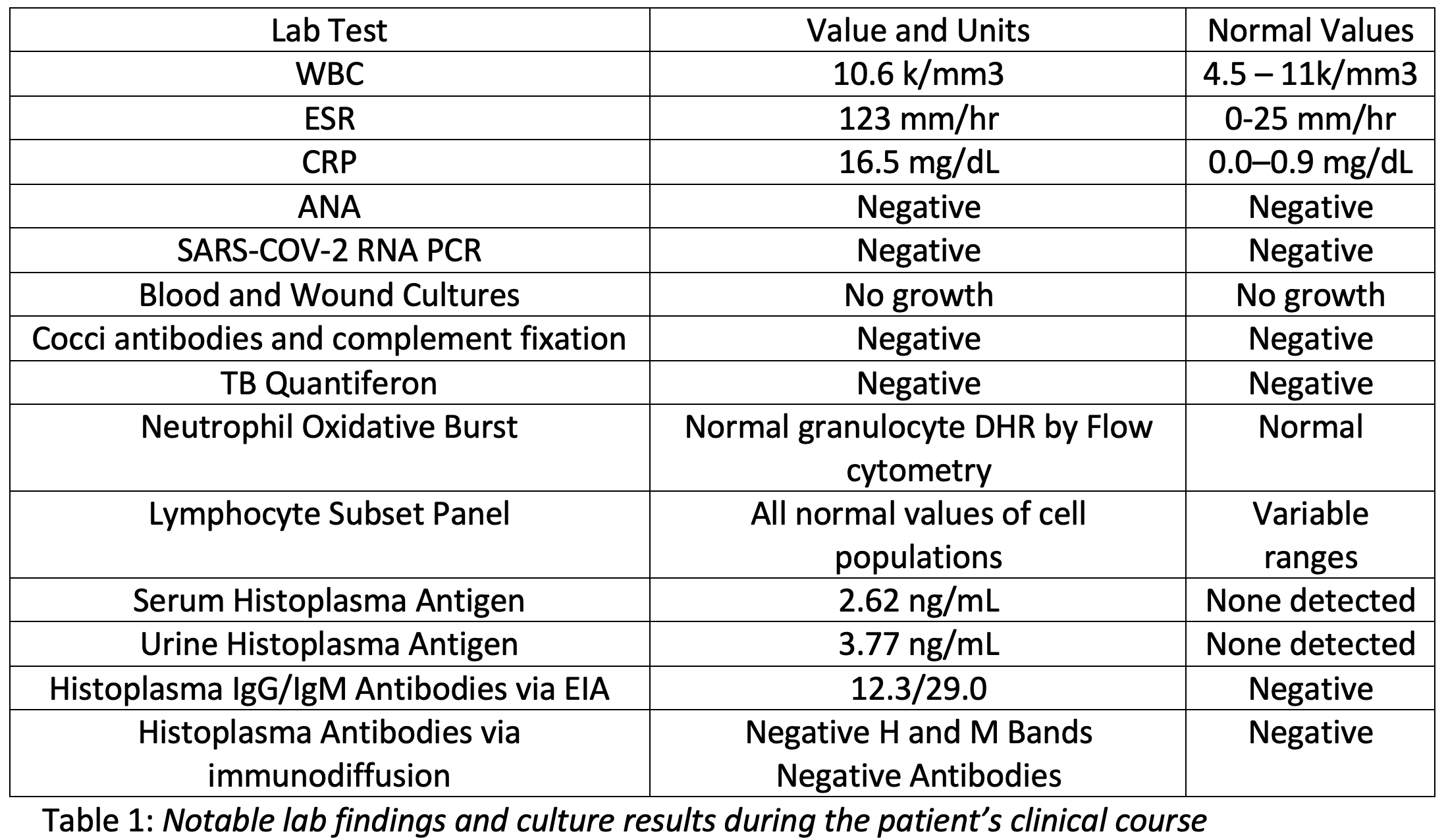
Case Presentation: A 17-year-old female was transferred from an outside hospital for persistent cough, infiltrate on chest x-ray (CXR), and draining nodules on her legs and back. 1 month prior to transfer, she developed cough, shortness of breath, and malaise without fever. A CXR was consistent with pneumonia and doxycycline was initiated. 5 days later she developed painful, erythematous nodules on her right leg, progressing over 2 weeks to her back, left leg, and hip. Ten days prior to transfer, her pediatrician changed her antibiotic to trimethoprim-sulfamethoxazole and sent wound cultures (negative). 1 week prior to transfer, the nodules began draining; she was admitted to an outside hospital. Repeat imaging confirmed a right lobar pneumonia and vancomycin and azithromycin were initiated. Notable lab work and studies are listed in Table 1. Skin lesion biopsies showed perivascular dermatitis with no panniculitis. Due to progression of skin lesions, she was transferred to a tertiary center. Upon transfer, VS and saturations were normal on room air. Physical exam revealed decreased aeration in the lung bases and multiple, painful, nodular lesions on both legs and back, some with serosanguinous and purulent drainage (Figure 1). Further testing, biopsies, and cultures were obtained (Table 1). Concern for endemic coccidioidomycosis was high and history of patient travel to Chicago prompted assessment for coccidioidomycosis and histoplasmosis. Histoplasma urine antigen was positive and preliminary skin biopsy results showed fungal elements; she was started on itraconazole for a planned duration of 1 year. Prior to discharge, her final culture results returned, confirming blastomycosis rather than histoplasmosis; no change in antifungal treatment was required. After discharge, she was followed weekly to monitor her skin lesions. 2 months after discharge, her skin lesions had fully healed and she remained symptom free.
Discussion: Blastomycosis is a granulomatous infection endemic to North America, specifically regions surrounding the Ohio and Mississippi River valleys and the Great Lakes. It presents as acute or chronic pulmonary disease and may disseminate to the skin, bones, or CNS. Diagnosis may be made by examination of wet mounts of sputum and culture confirmation is critical when possible. Serological testing may aid in the diagnosis but due to cross-reactivity with other fungi it cannot be relied on for a specific diagnosis. Dissemination occurs in roughly 15-20% of cases with a case fatality rate estimated between 4 – 6%. Though spontaneous resolution occurs in most children with pulmonary blastomycosis, treatment is recommended for all cases to prevent extrapulmonary dissemination. Given the nonspecific nature of this condition and its broad clinical manifestations, it has been described as “the great pretender”. Early diagnosis is essential to avoid disseminated disease and end organ damage.
Conclusions: This case highlights the importance of obtaining a thorough medical history and avoiding premature diagnostic closure. The initial presentation was suggestive of community acquired pneumonia and she was treated as such even after the eruption of her skin lesions, delaying initiation of appropriate treatment. Blastomycosis should be considered in any patient with nodular or ulcerated skin lesions and prolonged pulmonary symptoms unresponsive to antibacterial therapy who has residence in or history of travel to areas endemic for Blastomyces dermatiditis.