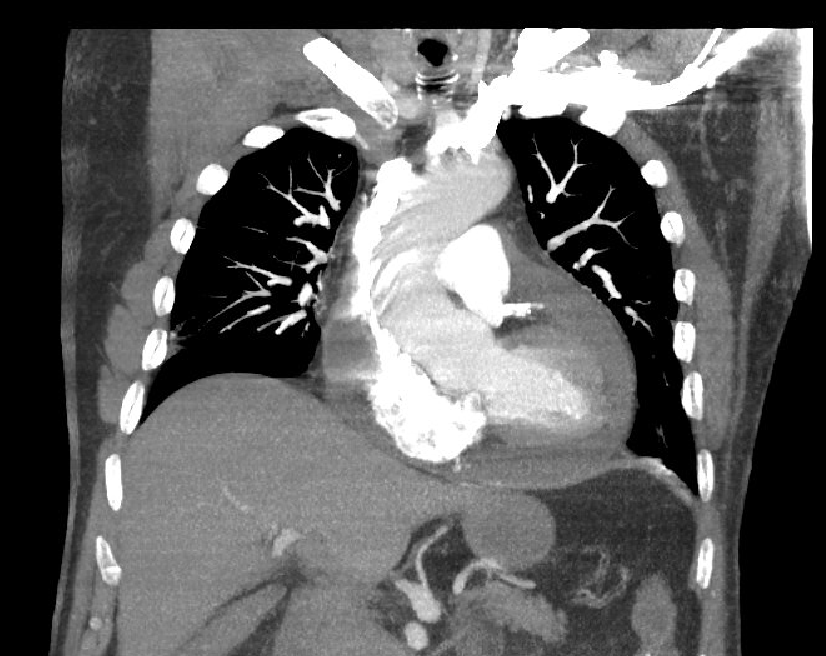
Case Presentation: 77-year-old Caucasian male presents to the ER due to progressive shortness of breath impacting his activities of daily activity. Shortness of breath started 2 weeks ago and was associated with a hacking cough and minimal sputum production for which he visited his physician’s office and received a steroid shot for “bronchitis”. On further review of symptoms, patient admitted to sharp back pains in the interscapular region that increased with deep inhalation which he attributed to his osteoarthritis. Pertinent physical exam findings included JVP on lower quadrant of neck and wheezing in bilateral lung fields on auscultation. Chest X ray on admission showed air space opacities, EKG recording was of low voltage. Provisional diagnosis of community acquired pneumonia (CAP) was made with initiation of antibiotic therapy. Due to clinical deterioration- worsening shortness of breath, a CT chest was done to evaluate the possibility of pulmonary embolism or aortic dissection. Echocardiogram done the next day concluded moderate pericardial effusion with signs of early tamponade, ejection fraction 50-55%. Indomethacin was initiated, and patient was scheduled for subxiphoid pericardial window later that day resulting in drainage of 440 ml of serosanguinous fluid, with complete resolution of symptoms.
Discussion: Physical findings associated with pericardial tamponade have varying sensitivity and specificity. Pulsus paradoxus has a sensitivity of 82%, specificity of 83%, was not performed. Beck’s triad of hypotension, dilated neck veins and muffled heart sounds were present in this case. This case highlights the contrast between an initial diagnosis of bronchitis followed by a diagnosis of CAP and the final diagnosis of pericardial effusion with early tamponade which could have been achieved earlier. Mycoplasma pneumoniae IgG antibodies were significantly elevated with normal IgM. A single reading of IgG antibody has low value (versus a single reading of IgM of 1:64 or greater, would have been diagnostic) in the diagnosis of Pneumonia due to Mycoplasma pneumoniae while a rising titer would have been more indicative of active infection. This laboratory result led to an early anchoring bias for initiation of antibiotics for CAP and delaying an evaluation which could have led the final diagnosis and limit the use of inappropriate antibiotics. Serology has significant limitation for diagnosis and should have been avoided. Treatment of pericardial effusion depends on its size and presence of signs of impending tamponade. Small or loculated effusion can be managed with pericardial window whereas a large effusion would warrant urgent pericardiocentesis.
Conclusions: Typical presentation of cardiac tamponade includes a recent predisposing condition and characteristic history and physical exam findings (e. g Pulsus paradoxus and Beck’s triad). Supportive and diagnostic findings include ECG with low voltage pulsus alternans, echocardiogram with swinging of heart within the effusion and diastolic collapse of right sided chambers. A history of bronchitis with an elevated IgG Mycoplasma antibody and early anchoring misled our initial clinical reasoning. If an echocardiogram had not been done (delayed due to lack of clinical suspicion) the diagnosis could have been missed. The importance of an initial comprehensive patient encounter along with awareness of cognitive biases in clinical reasoning cannot be overemphasized.