Background: Historically, patients transferred from one hospital to another are admitted through the emergency department and then placed on the desired unit at the accepting hospital. This practice creates delays for critically ill patients in need of continuous ICU care. A strategy known as the direct admission addresses this issue. With this strategy, transfer patients bypass the emergency department and are directly admitted to the desired unit at the accepting hospital. The current literature remains mixed in regards to the impact of this practice on patient outcomes such as mortality, length of stay, and 30 day readmission rate. Moreover, the financial implications of the direct admission are not well understood. Our purpose was to address this knowledge gap by analyzing cost and quality metrics for directly admitted MICU patients after our institution adopted this practice in 2016.
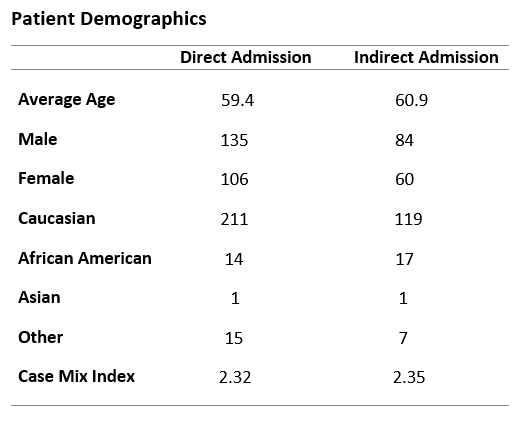
Methods: We performed a retrospective cohort analysis on MICU transfer patients admitted via the direct and emergency department routes. The cohorts were matched for patient characteristics such as age, race, gender, and case-mix index. Readmission and mortality rates were evaluated using a Chi-Squared analysis. Length of stay, hospital charge, cost of care supplies, and administrative costs were compared using an independent t-test with a 95% confidence interval and an alpha value of 0.05.
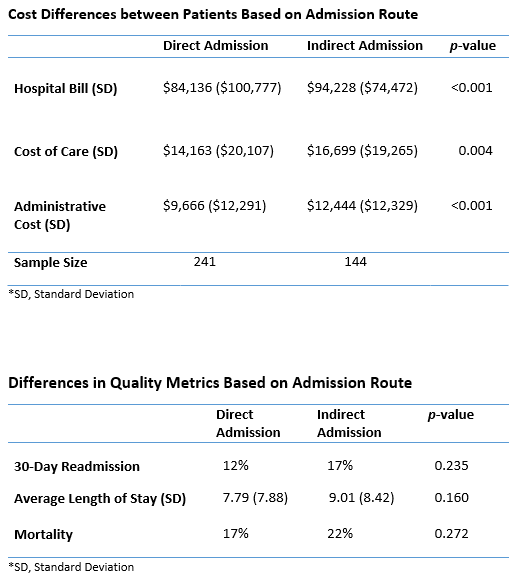
Results: Direct admission patients had significantly lower hospital charges when compared to indirect admission patients (p<0.001, direct 95% CI, $71,348-$96,924, indirect 95% CI, $81,961-$106,495). Direct admission patients also had significantly lower costs of care supplies when compared to indirect admission patients (p=0.004, direct 95% CI, $11,612-$16,714, indirect 95% CI, $13,526-$19,872). Lastly, direct admission patients had significantly lower administrative costs when compared to indirect admission patients (p<0.001, direct 95% CI, $8,106-$11,226, indirect 95% CI, $10,413-$14,475). Direct and indirect admission patients had an average LOS of 7.79 and 9.01 days, respectively, with a difference of 1.22 days. However, this difference was insignificant (p=0.160, 95% CI, -0.48, 2.93). The 30-day readmission rate for direct and indirect admission patients were 12% and 17%, respectively (p=0.235). Mortality rate for direct and indirect patients was 17% and 22%, respectively (p=0.272).
Conclusions: The direct admission model reduced hospital expenses for MICU transfer patients while having no impact on 30-day readmission rate, mortality, and length of stay. Hospitals should consider adopting the direct admission model, as it offers a more cost efficient approach to admitting transfer patients.