Background: Sleep is critical to children’s health and recovery, but pediatric inpatient sleep is often disrupted by nonessential overnight interruptions. The COVID-19 pandemic necessitated social distancing policies which minimized contact with low-risk patients. These policies have the potential to decrease overnight disruptions and improve sleep for hospitalized patients.
Methods: This cohort study compared sleep disruptions for pediatric inpatients admitted prior to (Sep 2018 – Feb 2020) and during (Apr 2020 – Aug 2020) the COVID-19 pandemic at a single site, urban academic medical center. Objective disruptions were measured as room entries detected by hand hygiene sensors for occupied rooms pre-pandemic (n_average=56) and during the pandemic (n_average=48) for 69 and 154 nights, respectively. Subjective reports of overnight disruptions, sleep quantity, and caregiver mood were measured by surveys adopted from validated tools: the Karolinska Sleep Log, Potential Hospital Sleep Disruptions and Noises Questionnaire, and Visual Analog Mood Scale. Caregivers of a convenience sample of pediatric general medicine inpatients completed surveys. Caregivers pre-pandemic were surveyed in person, and during the pandemic, surveys were conducted over the phone.
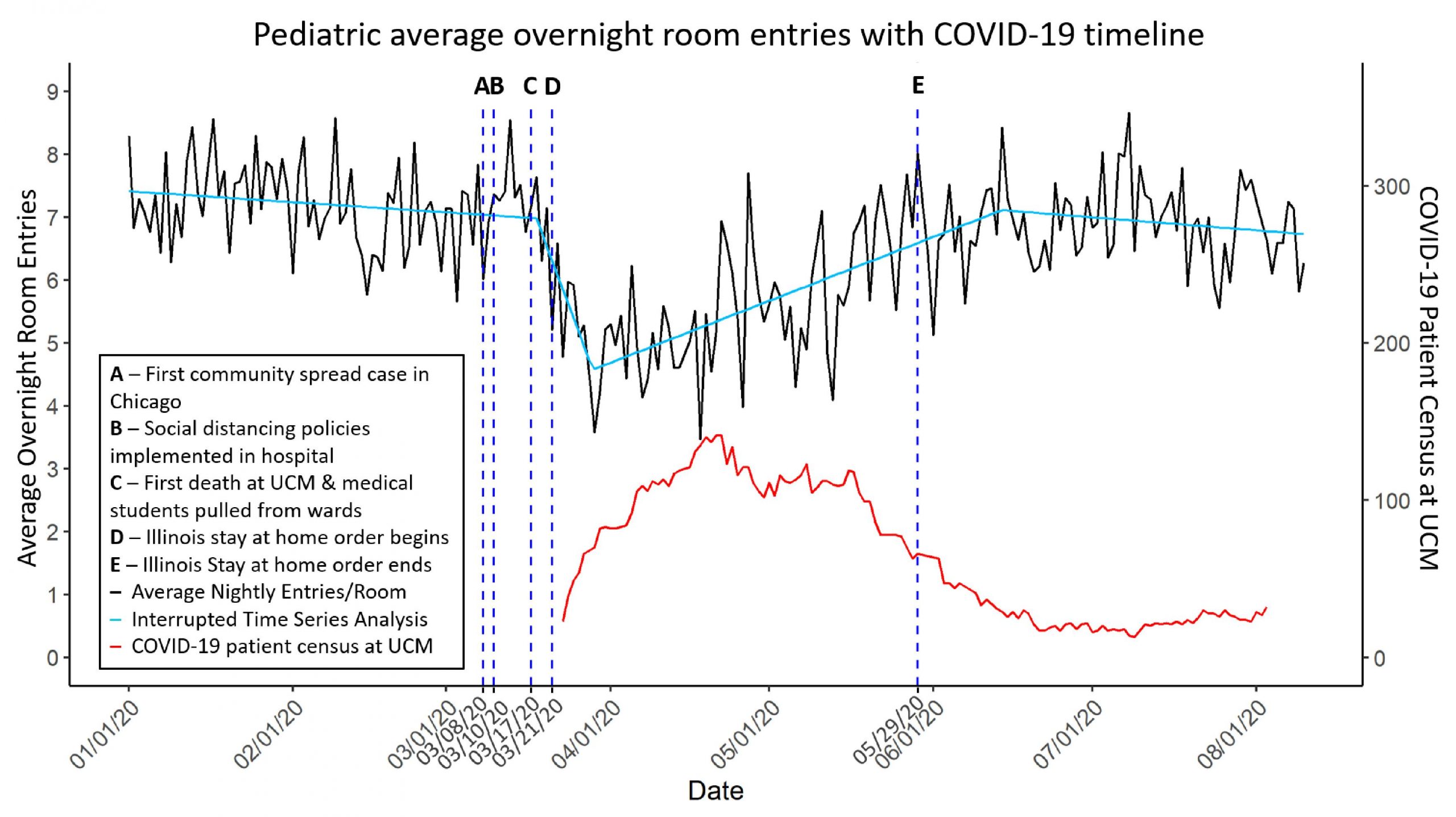
Results: 293 pre-pandemic (age_patients=4.1±4.4 years) and 154 pandemic (age_patients=8.7±5.6 years) surveys were collected from caregivers. The majority (71% pre-pandemic and 52% pandemic) of the study population identified as Black/African American. Nighttime room entries initially decreased 36% (95% CI: 30%, 42%, p<0.001), then returned towards pre-pandemic levels as the COVID-19 hospital caseload decreased. Despite this, caregivers reported more disrupted patient sleep (p<0.001) due to tests (21% vs. 38%) as well as stress (30% vs. 49%), anxiety (23% vs. 41%), and pain (23% vs. 48%). Caregivers also reported children slept 61 minutes less (95% CI: 12 min, 110 min, p<0.001) and had more awakenings. Caregivers self-reported feeling more sad and weary, less calm, and worse overall (p<0.001 for all).
Conclusions: Despite fewer objective room entries, caregivers reported increased sleep disruptions and an hour less nighttime sleep with more awakenings during the pandemic for pediatric patients. Caregivers also self-reported worse mood. This highlights the importance of addressing subjective perceptions and experiences of hospitalized children and their caregivers during hospitalization.