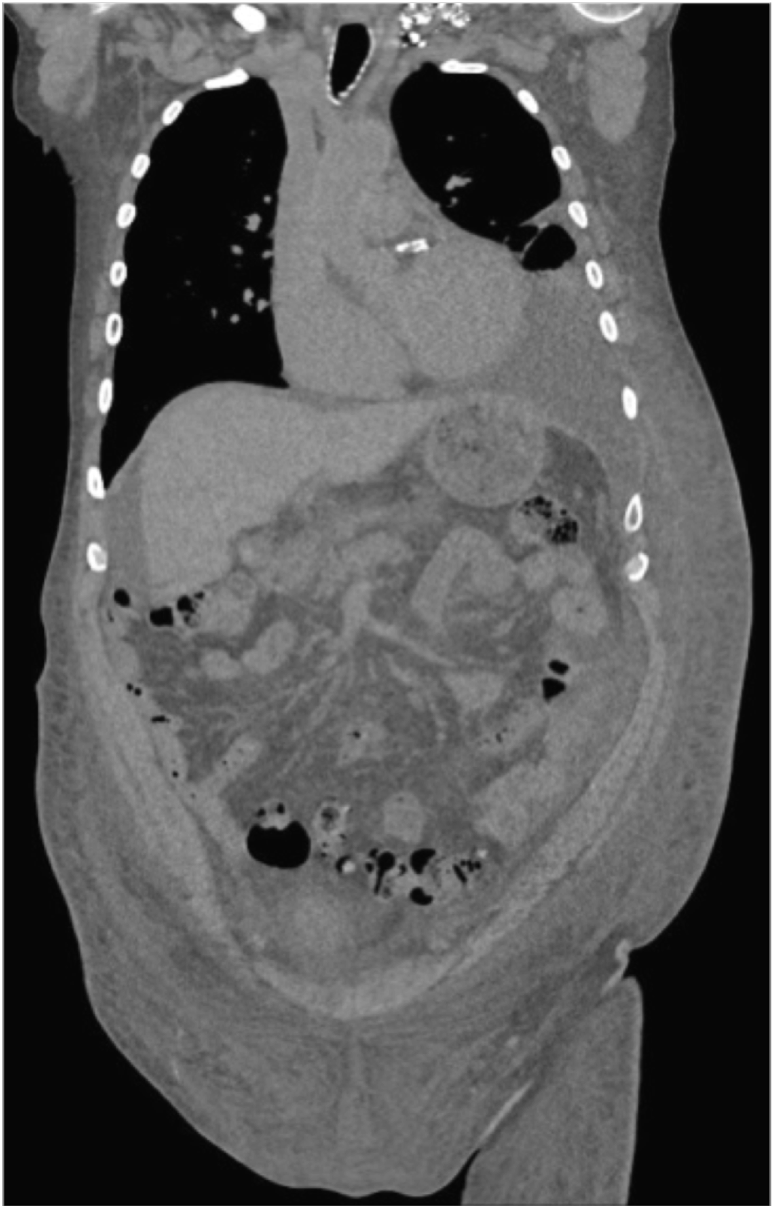
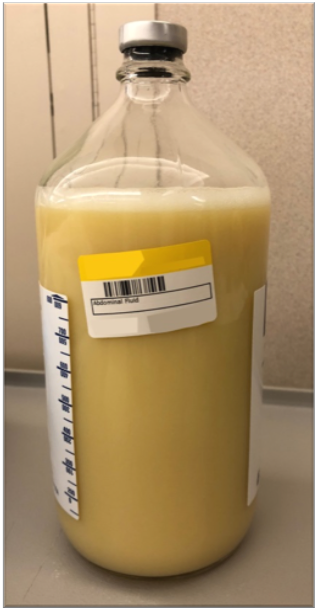
Case Presentation: A 70-year-old man presented with 5 months of anasarca and recurrent chylous ascites and left chylothorax. He had symptoms of dyspnea, orthostatic hypotension, bloating, early satiety, 20-pound unintentional weight loss, anasarca, and left periorbital purpura. He was a 25 pack-year current smoker with a past medical history including type 2 diabetes mellitus, hypothyroidism, and coronary artery disease status-post coronary artery bypass graft 2 years prior. Physical exam revealed left periorbital purpura, decreased breath sounds in left lower lobe, protuberant abdomen without tenderness, thickening of abdominal wall and skin of extremities with 3+ pitting edema to pelvis, with normal cardiac exam and no appreciable lymphadenopathy. Significant labs included hemoglobin 12.7, serum albumin 2.3, alkaline phosphatase 271, NT-proBNP 23,354 pg/mL, and high sensitivity troponin 189 ng/L. The total ascitic protein was 2.5, ascites albumin 1.0, with a serum-ascites albumin gradient (SAAG) of 1.3 The elevated SAAG and total ascetic protein of 2.5 suggested a cardiovascular etiology. Subsequent transthoracic echocardiogram revealed increased LV and RV wall thickness, biventricular systolic dysfunction, and strain pattern consistent with amyloidosis. Fat pad biopsy found a peptide profile consistent with AL (kappa)-type amyloid deposition, and liver biopsy showed amyloid deposition in portal tracts and vessel walls consistent with hepatic amyloidosis, but not meeting criteria for cirrhosis.
The patient was ultimately diagnosed with AL (kappa light chain) cardiac and hepatic amyloidosis. He was prescribed furosemide, spironolactone, midodrine, and cyclophosphamide-bortezomib-dexamethasone therapy, with a recommendation to follow a medium chain triglyceride diet and to take octreotide as temporizing measures to manage the ascites while awaiting the effects of treatment. The patient passed away 6 months after initial presenting symptoms.
Discussion: This case illustrates the utility of SAAG and total ascitic protein concentration to narrow the differential when complex patients present with chylous ascites and pleural effusion.
Amyloid cardiomyopathy is an uncommon disorder, with an incidence of 9 to 14 cases per million years in the United States. The disorder has high mortality rates, particularly in light-chain amyloidosis. Its non-specific symptoms and uncommon incidence make for a unique diagnostic challenge. The treatment of cardiac amyloidosis is twofold: therapy of heart failure and treatment of the underlying disease with chemotherapy; bortezomib-based regimens are first line therapy. Other regimens include melphalan with autologous hematopoietic stem cell transplantation.
Conclusions: Although uncommon, systemic amyloidosis is an important disease to consider in patients presenting with chylous ascites and pleural effusion, as recognition of this syndrome is critical to make a timely diagnosis and provide disease-directed therapy.