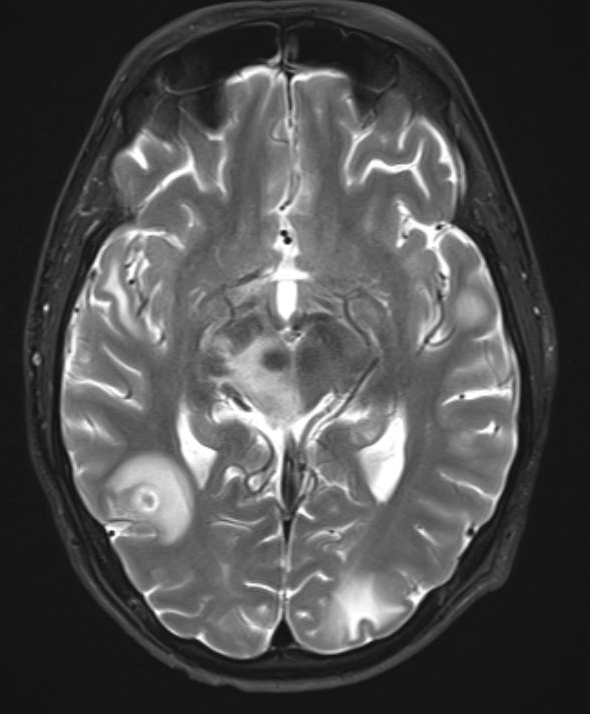
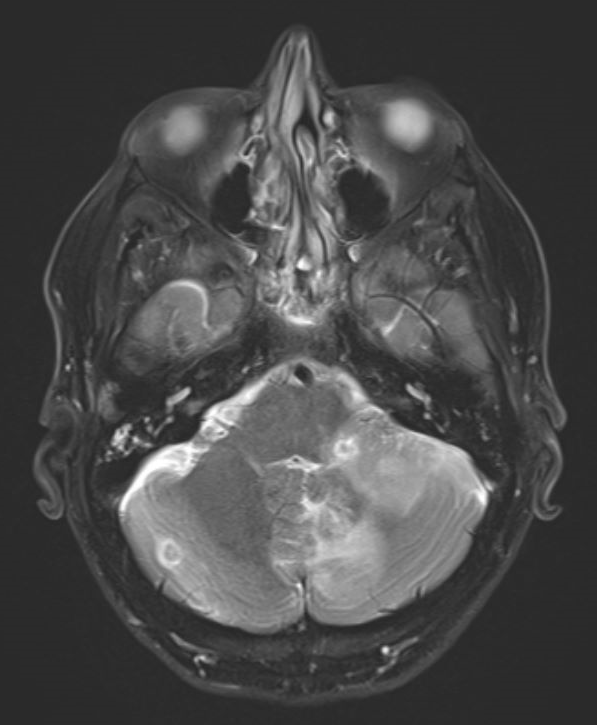
Case Presentation: A 49-year-old male with a history of type 1 diabetes mellitus, end stage renal disease, status post pancreas-kidney transplant maintained on tacrolimus and mycophenolate mofetil, who presented with a three-day history of fever, tension like headache, nausea, and non-bloody emesis. He denied exposures to pets, including cats. Laboratory values were significant for elevated white blood cell counts (WBC) of 13.5 K/uL, and a negative respiratory viral panel. Physical exam revealed fever of 39.5 C with a normal pulse and blood pressure. He was alert and oriented without any focal neurological signs, and with normal breath and heart sounds on auscultation. MR brain showed innumerable bilateral scattered ring-enhancing lesions compatible with a multifocal infection. A lumbar puncture was performed with cerebrospinal fluid (CSF) analysis showing leukocytes of 1005 cells/cmm (80% neutrophils), protein of 186 milligrams/deciliter and glucose of 63 milligrams/deciliter. He was started on ceftriaxone, vancomycin and ampicillin for bacterial meningitis. CSF cytology, bacterial and fungal cultures, and serologies (viral, cryptococcus, toxoplasma, histoplasma) were all negative. He became afebrile on day #3 of hospitalization. Due to the uncertain diagnosis, antibiotics coverages were changed multiple times but were eventually narrowed down to ceftriaxone given the negative studies and clinical response. Repeated CSF studies 12 days later showed improved WBCs of 56 cells/cmm (0% neutrophil, 85% lymphocytes) and protein of 82 milligrams/deciliter. CSF was sent for Metagenomic Next Generation Sequencing (NGS). Repeated brain MR after 2 weeks showed no interval changes. On hospital day #16 a brain biopsy was performed, which was negative for bacteria, fungi, acid-fast gram stains and cultures, unrevealing for a diagnosis. The patient continued to be afebrile and clinically improving. On hospital day #22, he was discharged home on intravenous ceftriaxone for presumed nocardia CNS infection. After discharge, NGS detected Bartonella Henselae by polymerase chain reaction (PCR). Antibody titers resulted in IgG of 1:1024. The patient was started on doxycycline. The diagnosis of Bartonella Henselae infection with brain abscesses was made.
Discussion: Bartonella infection (Cat Scratch Disease, CSD) is not uncommon infection, about 12,000 outpatient cases and 500 inpatient cases a year [1]. Most cases are mild and self-limited to cutaneous manifestation and regional lymphadenopathy, however, in severe cases, there are visceral organ, neurologic and ocular involvement. Our patient developed severe Bartonella infection with meningitis and multiple brain abscesses. His atypical presentation and lack of exposure history made the diagnosis very challenging. In our case, the CSF NGS played the major role for the diagnosis. Bartonella with CNS involvement usually presents with encephalopathy, aseptic meningitis, transverse myelitis and radiculitis [2]. Multiple brain abscesses have not been reported, although a case with brain granulomatous process was reported [3].
Conclusions: Bartonella infection could cause multiple brain abscesses in addition to meningitis. We report this case to heighten physicians’ awareness on Bartonella infection especially among immunocompromised and transplant population when presents with fever of unknown origin (FUO), meningitis and brain abscesses when no common pathogen could be found.