Case Presentation: Good’s syndrome (GS) is a rare, adult-onset combined B and T cell immunodeficiency with an associated thymoma. These patients have an increased risk of bacterial, fungal, viral, and opportunistic infections.
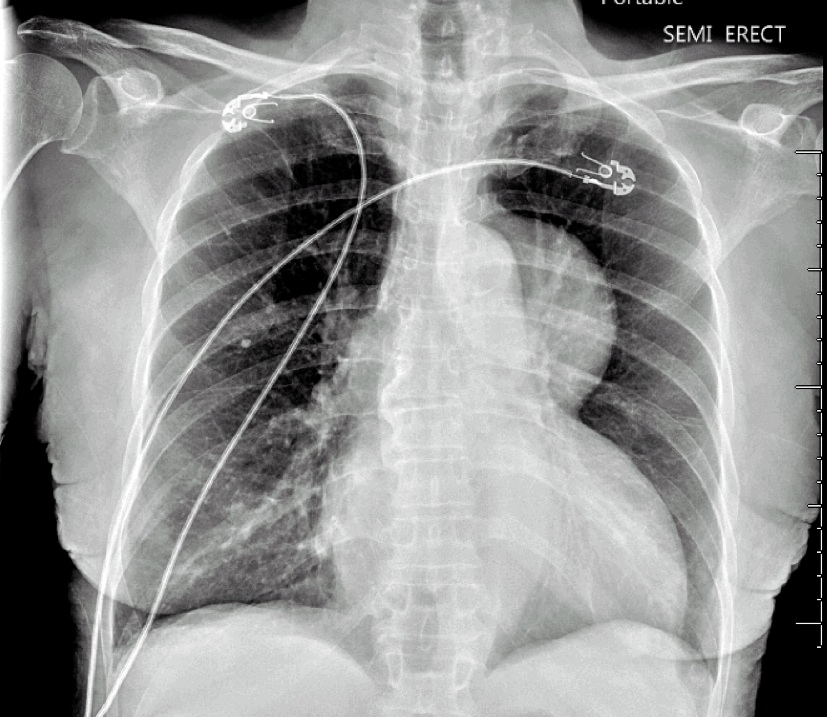
A 75-year-old African American female with congestive heart failure (ejection fraction 20%) and hypertension presented from home with a four-month history of fatigue, weight loss, and a full body desquamating rash, which began following an upper respiratory illness. On admission, her physical exam was notable for diffuse, darkened macules with a central targetoid appearance (Figure 1), oropharyngeal candidiasis, and 2+ pitting edema from her ankles to her knees bilaterally. She received a chest X-ray to complete an infectious work-up, which revealed an incidental anterior mediastinal mass (Figure 2). A follow-up Computed Tomography (CT) of her chest confirmed a 73.4mm x 87.1mm heterogeneous mass with scattered calcifications as well as enlarged bilateral axillary lymph nodes. She underwent a biopsy of her rash and mass, which demonstrated erythema multiforme and WHO Type A thymoma, respectively. During her hospitalization, she was also found to have oropharyngeal candidiasis, MSSA bacteremia and HSV-2 skin lesions. Based on the number of infections and severity of her rash, an immunocompromised state was suspected. Serum immunoglobulins were ordered, which demonstrated a low IgG (594) and a low IgM (19). Additionally, flow cytometry revealed a low CD4 count (175), confirming a combined B and T cell immunodeficiency. This combination of hypogammaglobulinemia and thymoma led to a diagnosis of GS.
Discussion: While GS does not have a formal diagnostic definition, it requires the presence of a thymoma, adult-onset immunodeficiency of CD4+ T-lymphocytes, mature B-lymphocytes, and hypogammaglobulinemia. As a result, these patients have an increased risk of recurrent sinopulmonary infections from encapsulated bacterial pathogens as well as viral and fungal infections. Of note, rates of opportunistic infections are higher in GS due to a loss of cell-mediated immunity. The exact pathogenesis of GS is unclear, but studies show that 87% of cases have reduced mature B-cells and pre-B cells in the bone marrow, indicating a myelosuppressive process believed to be secondary to cytokine inhibition or autoantibody production. GS typically presents in the sixth decade of life and has equal incidence between males and females.
Conclusions: GS should be suspected in patients older than 40 who present with new opportunistic infections, absent or reduced serum immunoglobulins, and recurrent sinopulmonary infections. All patients with thymomas should undergo immunoglobulin testing, receive appropriate prophylactic antibiotics and be evaluated for thymoma resection.