Background: Evidence-based guidelines/protocols for electrolyte replacement that safely encourage oral (PO) and/or intravenous (IV) dosing attain goal levels more successfully than standard care.1-17 PO is generally more comfortable and less dangerous than IV. Between 5/2017-11/2017, Jefferson dosed ~300,000 doses of potassium (K) and magnesium (Mg), with 30% and 19% of doses being PO, respectively. Guiding clinicians to evidence-based repletion that encourages PO may improve repletion success, patient satisfaction, reduce pain, save cost, and reduce need for telemetry monitoring.
Methods: We created a multidisciplinary team and completed a literature review to update our guidelines. Goals included renal dosage adjustment, administration-route and formulation-choice suggestion based on clinical status, telemetry monitoring and nephrology consult guidance, and clear guideline-use exclusions. We also sought to include situational awareness and utilized behavioral economic “nudge” theory into the orderset to improve patient care while reducing provider cognitive load. As previously described through numerous iterative improvements we were able to increase orderset utilization and percentage of PO dosing. To evaluate efficacy, 400 patients (100 patients in each pre-post K/Mg subgroup) were manually reviewed for repletion within normal limits (WNL), within goal (3.9-4.3 mmol/L, K; >2 mEq/L, Mg), and above threshold for telemetry per American Heart Association (AHA) guidelines. Cost impacts were extrapolated from institutional cost data.
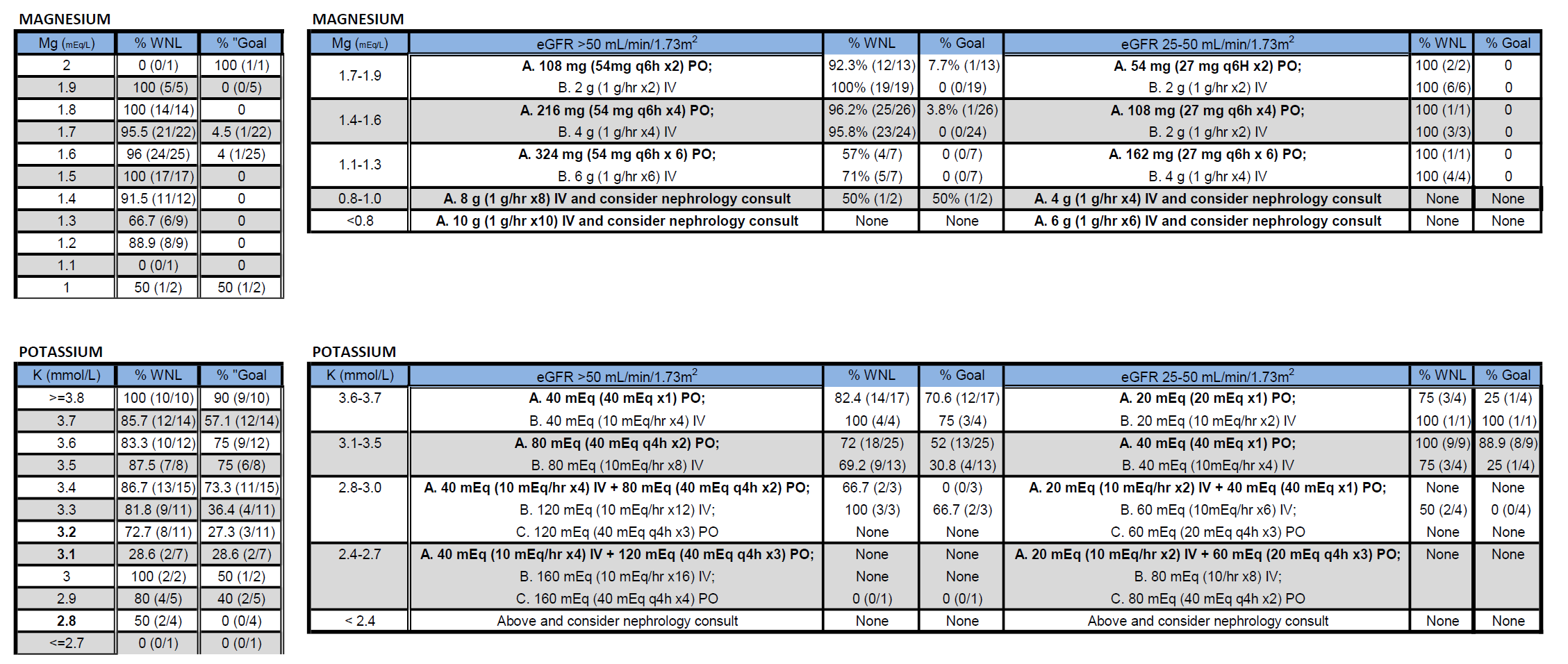
Results: Relative to prior care, the guideline-based repletion significantly improved repletion WNL, to goal, and outside of AHA telemetry thresholds. (Figure 1) Specifically, K and Mg repletion WNL rose from 58.3% to 79.0% and 75.0% to 91.5%, respectively (both p< 0.05). The component PO and IV repletion changes trended toward improvement: PO K 70.2%->81.3%, IV K 58.5%->77.4%; PO Mg 77.8%->90.2%, IV Mg 74.7%->92.4%. Post-repletion K or Mg levels requiring telemetry per AHA guidance dropped from 7.3% to 2.3% (p< 0.05). There were no over-repletion nor rescue medication events. On guideline, repletion success by route, renal-impairment, and baseline electrolyte level varied from 0-100% as detailed in Figure 2.The combination of improved percentage of PO dosing and on-guideline improved repletion efficacy extrapolates to 906 (2,413 if there is universal guideline adherence) patients/year avoiding cardiac arrhythmia risk per AHA guidance; 5,877 (14,366) fewer annual doses of unnecessary, potentially painful IV K; less time connected to IV poles and/or telemetry; and fewer repeat repletion doses. From a systems standpoint, this leads to $79,633 ($209,783) annual medication acquisition cost savings, $45,334 ($120,683) telemetry savings, and potential for reduced boarding time and improved patient satisfaction.
Conclusions: An evidence-based K/Mg repletion guideline and accompanying orderset significantly improves repletion efficacy across several domains. Given no over-repletion, we will improve repletion WNL, to goal, and out of high-risk zones by increasing K and Mg dosing by level. This is one of the first studies to demonstrate efficacy in a non-ICU setting. As it demonstrates specific repletion efficacy and resultant patient, cost, and systems benefits we suggest other institutions adopt a similar approach to pave the way for high-value, safe, patient-centered electrolyte repletion.