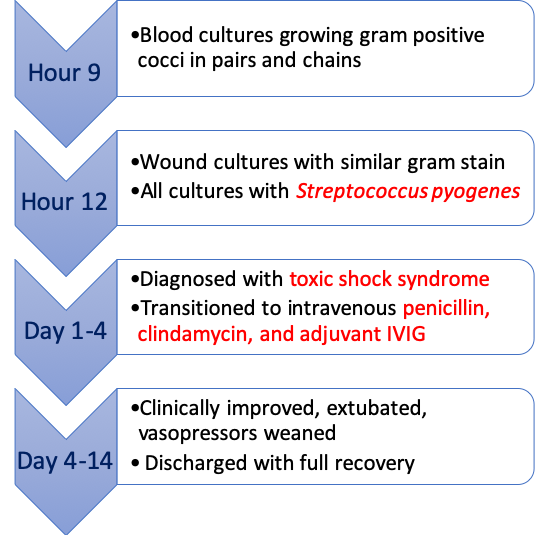
Case Presentation: A 40-year-old Caucasian woman with history of surgically-repaired lumbar spinal stenosis presented with a progressive swollen and painful right foot over past few hours. The patient was concerned of a spider bite though did not see a spider. The dorsal aspect of the foot was erythematous, edematous, with a pinpoint area of necrosis and exquisitely tender. CT imaging showed soft tissue swelling without fluid collections or gas, and without any signs of necrotizing fasciitis. The patient was given a test dose of equine serum followed by black widow spider antivenin, which she initially tolerated. However, over the course of one hour she rapidly became febrile to 103F and hypotensive with blood pressures in the 60s/40s. She was started on intravenous epinephrine for possible anaphylaxis, needing two additional vasopressors for blood pressure support. She was given intravenous fluids and started on vancomycin, piperacillin-tazobactam and clindamycin. Repeat bedside surgical evaluation demonstrated superficial skin necrosis without deep necrotizing soft tissue infection. Repeat laboratory testing demonstrated rapid onset acute kidney injury (creatinine: 0.5 to 1.2), elevated liver enzymes (transaminases: low 100s), thrombocytopenia (platelets: 205 to 43) and lactic acidosis (lactate: 9). The patient eventually required intubation given worsening respiratory status. Nine hours after admission, blood cultures showed growth of gram-positive cocci in pairs and chains, with similar growth thereafter in wound cultures. The species was subsequently identified as Streptococcus pyogenes. The patient was finally diagnosed with streptococcal toxic shock syndrome, and was treated with intravenous penicillin, clindamycin and adjunctive intravenous immunoglobulin. The patient’s condition improved, and she was ultimately discharged with near full recovery.
Discussion: Initially the patient’s symptoms raised concern for a black widow bite even though these bites are rare, seldom cause infection, and are not associated with tissue necrosis. Subsequently, it became apparent that the patient’s overall condition was inconsistent with the initially suspected etiologies of bite, cellulitis or deep tissue infection. The patient was astutely started on broad-spectrum antibiotics with appropriate dosing and coverage for toxic shock syndrome almost a half-day prior to the definitive diagnosis. While rare, occurring in approximately 3.5 cases per 100,000 persons, rates of invasive group A streptococcal infection have increased steadily in North America over the past decades for yet-unclear reasons. With mortality rates as high as 60%, recognition of this potential diagnosis early and knowledge of the clinical criteria for diagnosis is critically important in caring for these patients.
Conclusions: Consider life threatening condition like Toxic Shock Syndrome in seemingly uncomplicated insect bites or cellulitis with unexpected deterioration.