Background: Preliminary data from the 2018 Clerkship Directors in Internal Medicine (CDIM) survey showed that in about 50% of both academic and community medical centers, medical students rotate directly with attendings (1). This number has increased by 400% from 2010, the last year for which data is available (2). In our institution, hospital medicine (HM) faculty have the opportunity to rotate on both a traditional team teaching model (TTTM), consisting of interns and residents, and a direct care apprenticeship model (DCAM), where they are paired directly with third year internal medicine (IM) clerkship students. Students on DCAM rate the same attendings more poorly than when they attend on TTTM (3). Our faculty have expressed anecdotal dissatisfaction with their role in DCAM, often opting out of this teaching format (4). Accordingly, we sought to better understand the faculty experience on DCAM.
Methods: We surveyed faculty in our HM group who rotated on DCAM to assess the perceived time commitment, their perception of barriers to success, overall satisfaction, their relationships with students, burnout, and effect on career interest. We also sought to better understand the time they spend in clinical care and various aspects of teaching while on DCAM. For faculty who also rotate on TTTM, we sought to understand and compare faculty perceptions of time commitment while on TTTM.Means and standard deviations were used to analyze continuous variables. Two-tailed t-tests were used to compare continuous variables. A p-value of <0.05 was considered significant.
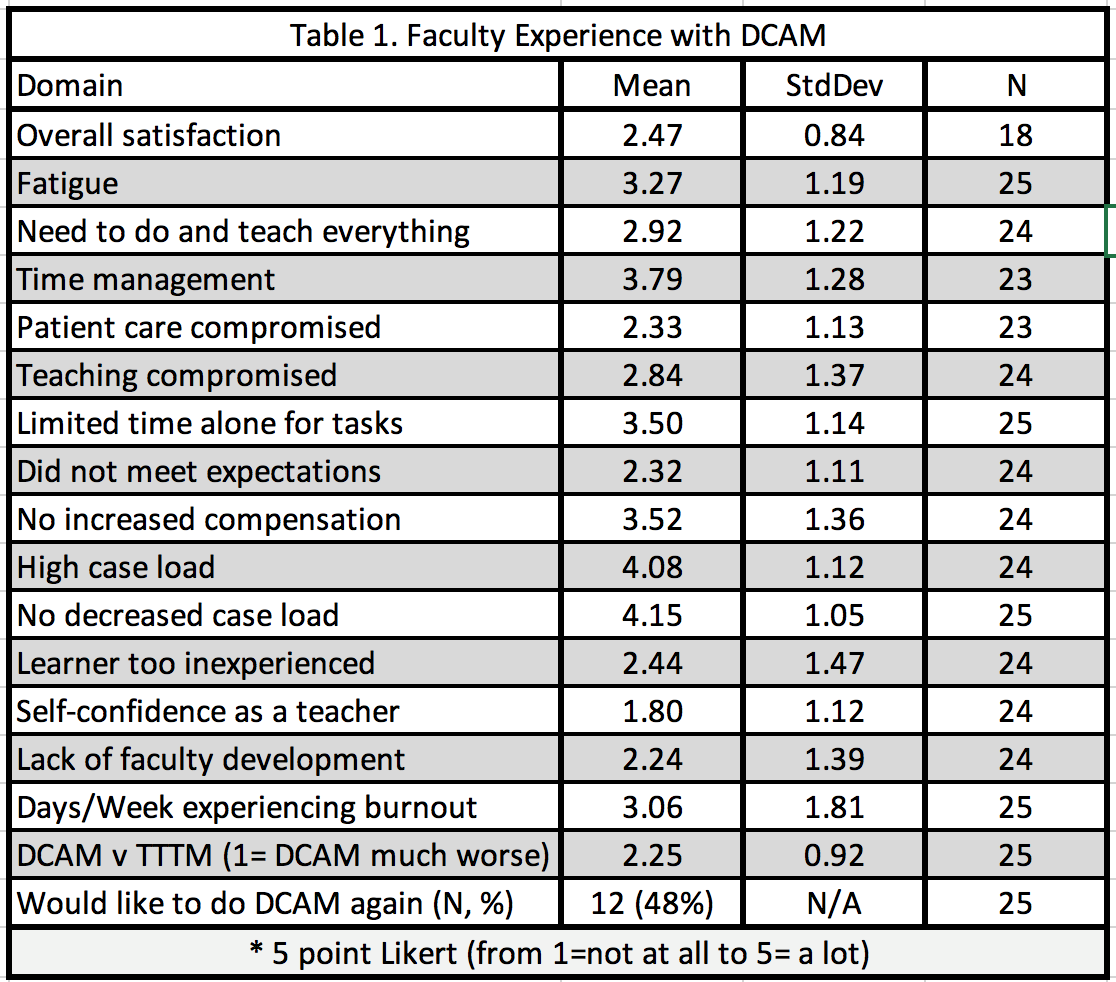
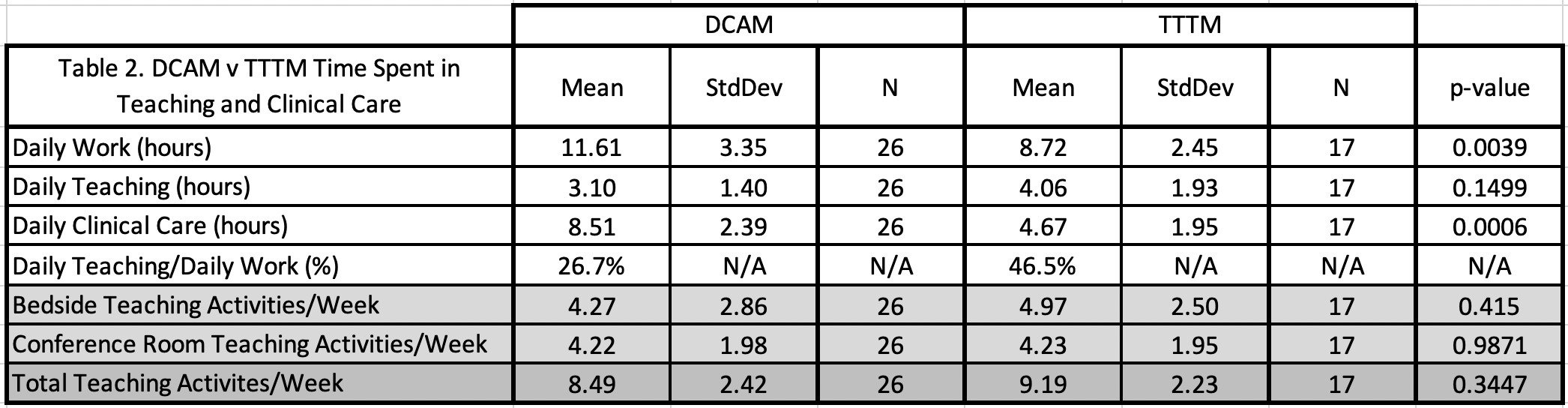
Results: 27 of 40 (68%) faculty members who attend on DCAM completed the survey.Faculty indicated that on DCAM, they struggled more with a high census, an inadequate reduction in case load, time management, and limited time alone to accomplish tasks (Table 1). Overall satisfaction with DCAM pointed towards dissatisfaction with a mean of 2.47 on a five-point Likert scale where 1 is not at all satisfied. On an average of 3.06 days a week (43.7%), our faculty experience burnout while teaching in DCAM. Less than half (48%) of our faculty indicated they wished to continue teaching in DCAM. Faculty found DCAM to be less rewarding than TTTM (mean of 2.25, SD 0.92).In DCAM, our faculty work 33.1% more time daily (11.61 hrs/day versus 8.72 hrs/day, p=0.0039) (Table 2). We found no significant difference in time spent teaching students between DCAM and TTTM attendings, nor was there a significant difference in episodes of teaching, whether at bedside or in conference rooms. However, DCAM attendings spend 82.4% more hours a day in direct clinical care as compared to TTTM attendings (8.51 hrs/day v 4.67 hrs/day, p= 0.006). This amounts to DCAM faculty spending nearly 3 hours (2.89 hrs) (p=0.0039) a day more of total hours at work and almost 4 hours (3.84 hrs) a day more in clinical care (p= 0.006). DCAM faculty spend only 26.7% of their time teaching, while on TTTM, almost 46.5% of the day is spent teaching.
Conclusions: Attendings work nearly 12 hours daily while on DCAM, almost 3 hours a day more than when they are attending on TTTM. Despite this, our faculty continue to prioritize teaching. We found no significant difference in either teaching time or weekly teaching episodes between DCAM and TTTM. In light of the increased workload and evidence that DCAM may be contributing to burnout and job dissatisfaction, survey results suggest that increased compensation, a proportionate decrease in case load, and/or a more efficient workflow should be considered for faculty on DCAM.