Background: Alcoholic hepatitis (AH) related admissions have been increasing, and severe AH (as defined by a discriminant function [DF] > 32) can carry a one-month mortality rate of up to 50% (Crabb et al). With rising mortality from alcoholic liver disease, early detection of alcohol use disorder to achieve cessation and prevent progression to alcoholic cirrhosis has been recognized as a critical intervention (Moon et al). AH therefore necessitates timely diagnosis, work up and treatment to reduce morbidity and mortality. Diagnostic errors due to cognitive heuristics have also been increasingly emphasized (Croskerry). The prevalence and outcomes of undiagnosed, untreated AH in hospitalized patients is unknown. As part of a hospital medicine (HM) – hepatology collaborative to optimize the care of patients with AH, we aimed to quantify the prevalence of unrecognized AH cases on our HM service and assess the effects of under recognition on processes and outcomes of care.
Methods: We performed a retrospective cohort study of patients admitted without hepatology consultation to the HM direct care service of Parkland Memorial Hospital from July 1, 2018 to June 30, 2019. For patients with elevations in both AST and ALT in a greater than 1.5:1 ratio and documented heavy alcohol use (by ethanol level or by history), charts were reviewed to determine if the diagnosis of alcohol-related hepatitis was present. Demographics as well as processes and outcomes of care metrics for AH patients were abstracted. Two sided t-tests were used to compare continuous variables and chi-square tests were used to compare categorical variables. SAS version 9.4 was used for all analyses. P-values of < 0.05 were considered significant.
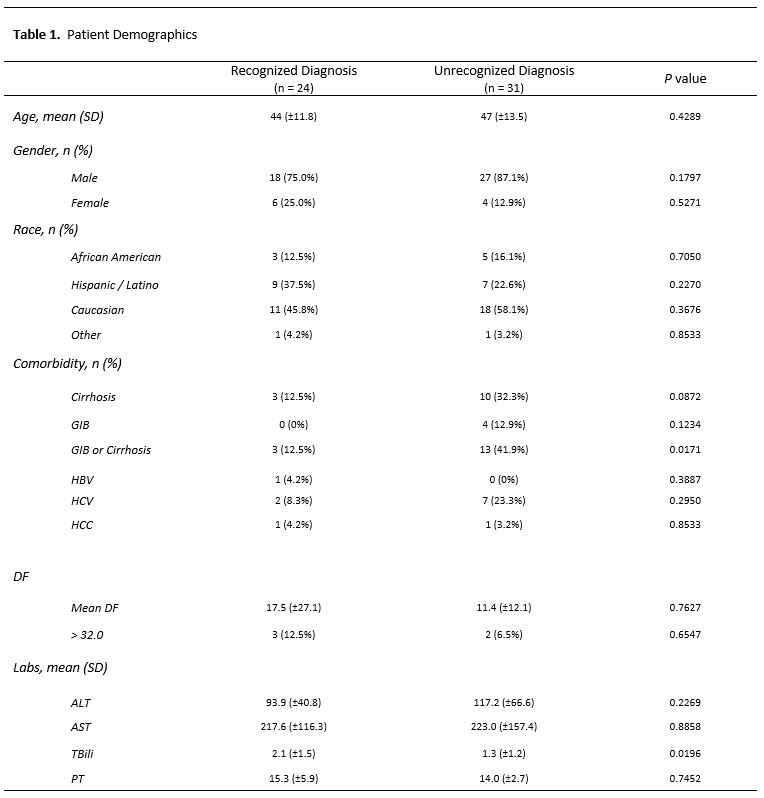
Results: 24 recognized and 31 unrecognized AH patients were identified. Patients under both subsets had similar demographics and comorbidities (Table 1). The mean DF was not significantly different between cohorts; however, 3 patients in the recognized cohort and 2 patients in the unrecognized cohort had DFs >32. Patients with recognized AH had a lower incidence of cirrhosis or GIB (12.5% vs 41.9%, p=.02), higher total bilirubin levels (2.1 vs 1.3, p=0.02) and received blood cultures more often (46% vs 19%, p=.03) than patients with unrecognized AH. 2 patients in each cohort met treatment criteria for steroids, but neither in either subset received steroids (Table 2).
Conclusions: There were 31 cases of undiagnosed AH on our HM direct care service without hepatology consultation out of the 20,075 admissions to the HM service during the year studied, resulting in an overall prevalence of 1.54 unrecognized AH cases/1000 admissions. This is very low and only 2 cases of severe AH were unrecognized, which may be a reflection that the majority of AH cases, especially severe AH, are co-managed with hepatology. Unrecognized AH patients tend to have less severe disease, perhaps leading to lack of recognition due to base rate neglect. Additionally, the higher incidence of cirrhosis or GIB in unrecognized AH cases may indicate an anchoring or blind spot bias. Unrecognized, mild and moderate AH may represent a missed opportunity for continued disease monitoring and additional alcohol cessation counseling. Natural language processing and artificial intelligence as diagnostic aids may help to even further reduce the already low prevalence of unrecognized AH to aid in early diagnosis for all patients and eliminate missed severe, treatable AH.