Background: Clinicians are not always effective communicators. Communication skill training provided to students, fellows, and faculty is inconsistent.1 However, system-wide relationship-centered communication skills training can improve patient satisfaction scores, reduce burnout, and improve physician empathy.2 Thus, our study’s objective was to determine if a voluntary one-day skills-based communication course could improve provider knowledge, confidence, and patient experience scores.
Methods: In this longitudinal study initiated in 2017, we assessed the impact of the Utah Advanced Communication Training (UACT) Program for health care providers. UACT is an 8-hour skills course that expands healthcare providers and staff’s communication skills. Between 2017 and 2019, UACT was offered nine times. Participants were were surveyed on communication knowledge and confidence immediately before and after the course. In addition, we collected patient experience scores using medical practice survey data which included 11 different questions and was sent to patients after their outpatient visit. Provider-specific patient experience scores were averaged based on time point and question and categorized into six 3 month quarters (1-pre course and 5-post course). To assess differences in pre versus post-UACT participant responses, we used 2-tailed T-tests. To assess the mean difference in inpatients’ experience scores for each question, we used nested mixed-effect linear regression models comparing pre-course and post-course scores. The University of Utah IRB approved this study under non-human subject research.
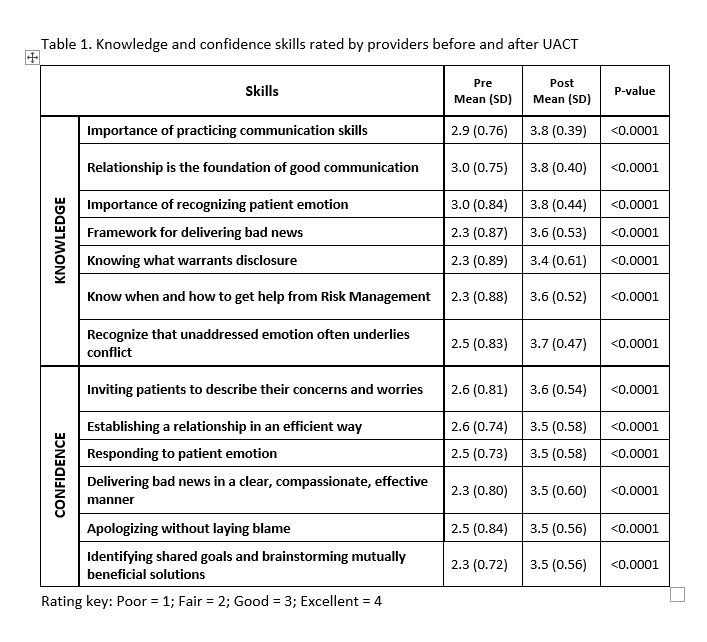
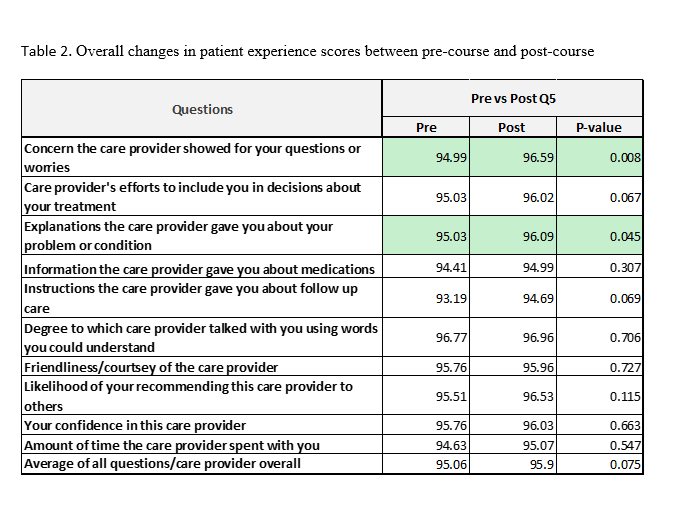
Results: A total of 142 health care providers and staff consisting of physicians, advanced practice clinicians, registered nurses, and other multidisciplinary team members participated in the clinical skills training over two years. Survey completion rates were 75% for the pre-survey and 68% for the post-survey. Thirty-two providers were included in the analysis of patient experience scores based on sufficient patient survey response rate (>30 surveys). Differences in pre and post-UACT participant survey results are shown in Table 1. UACT participants reported significant improvement in all areas of communication knowledge and confidence. No significant differences were seen in patient experiences scores until 13 months after the course (post-Q5). During this 3 month period, we did see a statistically significant difference in patients’ mean scores for the statements “concern care provider showed for your questions and worries” and “explanations the care provider gave you about your problem or condition,” indicating a potential late effect of the intervention (Table 2).
Conclusions: We found improvement in patient experience and participant knowledge and confidence following an 8-hour communication skills course. In the hospital, emotions often run high and having skills to establish rapport quickly and descalate conflict is critical. Communication is vital to the patient-provider experience, and a short skills-based course can help set the foundation to give practitioners tools to improve their confidence with difficult conversations. As these difficult conversations are becoming more common in the era of COVID, our goal is to expand UACT to an online platform to allow more accessibility.