Background: Patients with COVID-19 have increased rates of venous thromboembolism, however, there is currently no standardized approach to anticoagulation (AC) therapy particularly with respect to the proper dose of anticoagulation (prophylactic or therapeutic). Many observational studies have shown a mortality benefit in using prophylactic AC for hospitalized patients with COVID-19. A few studies have reported increased rates of bleeding with therapeutic dose AC compared to prophylactic dose AC, yet there is limited evidence on the association of therapeutic AC with other adverse outcomes. The purpose of this study was to characterize anticoagulation use in patients with COVID-19 and to examine the association of therapeutic AC with other hospital complications including blood transfusion and acute drop in hemoglobin or platelet count.
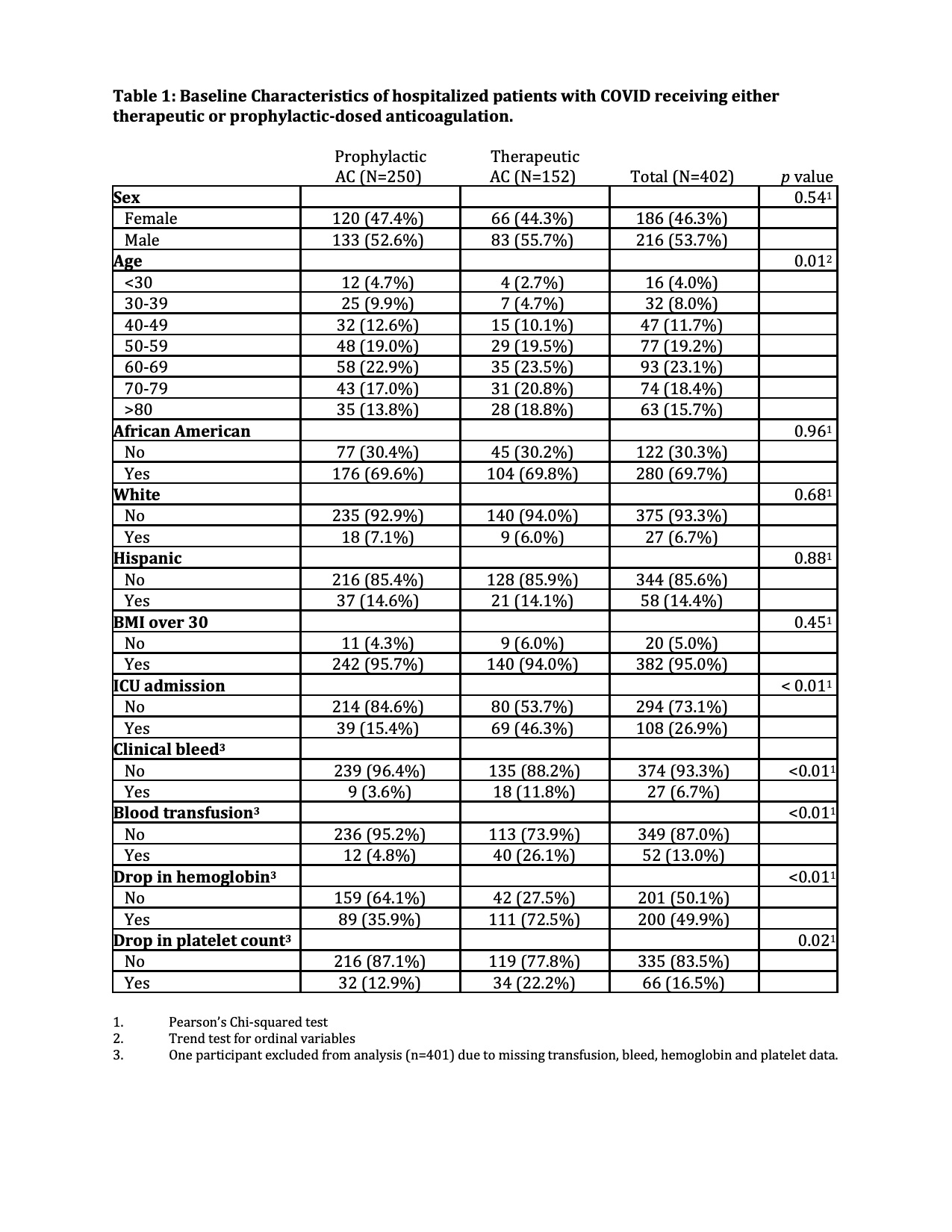
Methods: A single-center retrospective analysis was conducted on patients hospitalized between March 15, 2020 and May 31, 2020 with a confirmed diagnosis of COVID receiving either therapeutic or prophylactic-dosed anticoagulation (with IRB approval, NCR202580). Initial descriptive statistics were used to summarize basic patient population characteristics. We performed univariate logistic regression and chi square analysis to study the odds of clinical bleed, platelet decrease greater than 50%, hemoglobin drop greater than 2g/dL and need for one or more packed red blood cell transfusion with respect to therapeutic anticoagulation. We completed a subsequent sub-analysis stratified by ICU admission status.
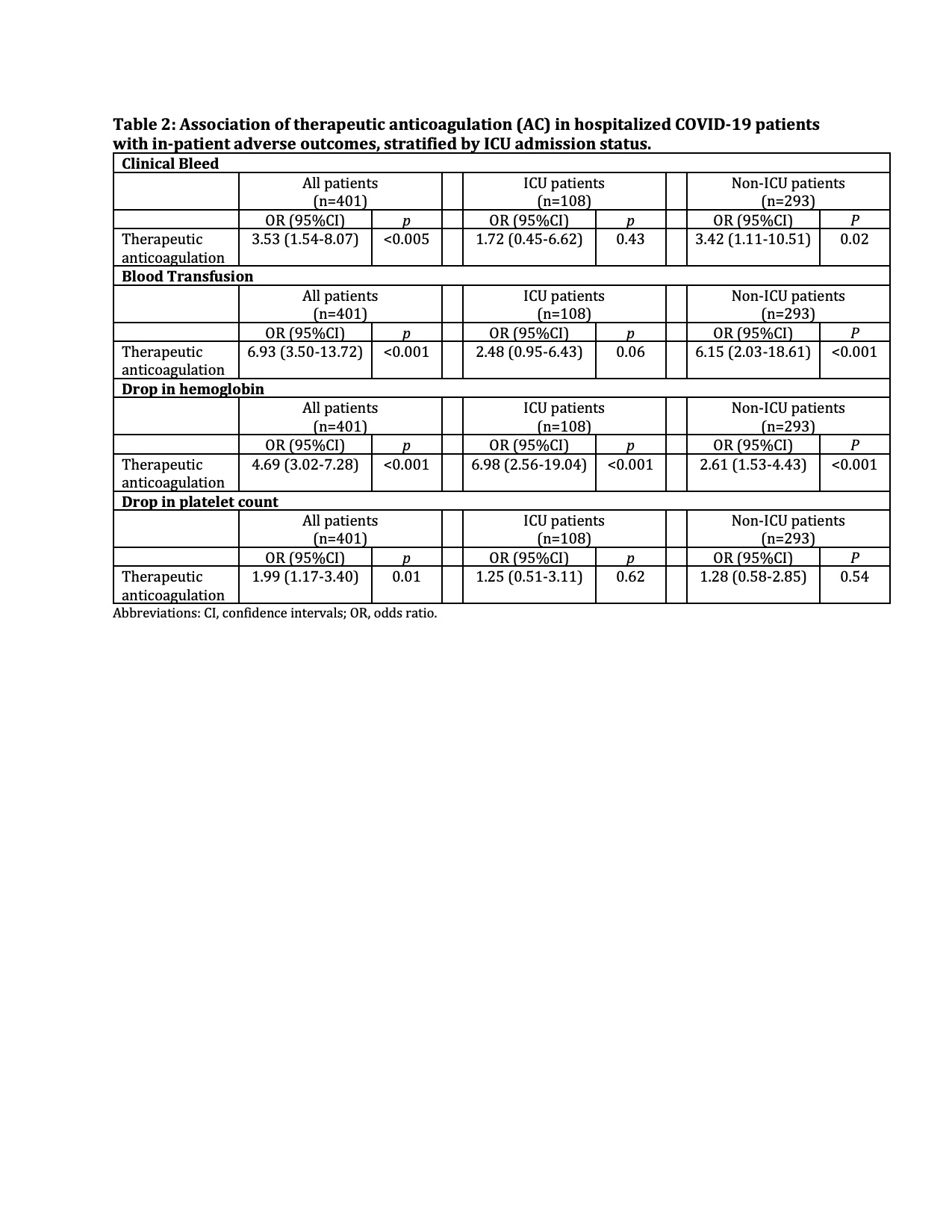
Results: Of the 402 patients included in analysis, median age was 63 years, 69.7% African American, 95.0% had a BMI greater than 30, and 26.9% required ICU admission. 38.3% of patients were placed on therapeutic anticoagulation vs. 61.7% on prophylactic anticoagulation. Overall, blood transfusion rate was 13.0% while clinical bleeding rate was 6.7%. Finally, 200 patients (49.9%) had an acute drop in hemoglobin greater than or equal to 2 g/dL while 66 patients (16.5%) had a decrease in platelet count of at least fifty percent during their hospital-stay. From univariate logistic regression analysis, compared to those on prophylactic AC, therapeutic AC was significantly associated with increased odds of clinical bleed (odds ratio (OR): 3.53, 95%CI: 1.54-8.07, p <0.005), drop in hemoglobin (OR: 4.69, 95%CI: 3.02-7.28, p <0.001), drop in platelet count (OR: 1.99, 95%CI: 1.17-3.40, p = 0.01), and blood transfusion (OR: 6.93, 95%CI: 3.50-13.72, p <0.001). In the subsequent stratified analysis, therapeutic anticoagulation remained significantly associated with hemoglobin drop and blood transfusion independent of ICU admission status. Among non-ICU admitted patients, odds of clinical bleed were 3.42-fold more likely in patients on therapeutic dose anticoagulation compared to patients on prophylactic dose anticoagulation (95%CI: 1.11-10.51, p = 0.02).
Conclusions: Hospitalized patients with COVID-19 placed on therapeutic anticoagulation were more likely to have a clinical bleed, require a blood transfusion, or have an acute drop in hemoglobin or platelet count compared to patients placed on prophylactic anticoagulation. Each of these inpatient complications could affect clinical decision making, including early cessation of AC, increased blood laboratory testing, and increased hospital length of stay. These data may be used to inform future randomized trials needed to determine optimal AC therapy in hospitalized patients with COVID-19.