Background: Altered mental status (AMS) is prevalent in hospitalized patients, especially the elderly (1). The work up of AMS is based on history, physical exam, pertinent labs and imaging. Common etiologies include fluid and electrolyte disturbances, infections, drug toxicity, drug withdrawal and metabolic derangements. Many routine labs drawn in the evaluation of acute encephalopathy are more suited to work up for sub-acute or chronic neurocognitive declines. Vitamin B12 deficiency and thyroid derangements cause cognitive disturbances which are mostly insidious in onset. Folic acid has low clinical utility, even in the work up of dementia. The utility of an RPR screening for neurosyphilis as a cause for AMS is unknown. Accordingly, we sought to evaluate the yield of B12, folate, TSH and RPR testing in hospitalized patients with AMS.
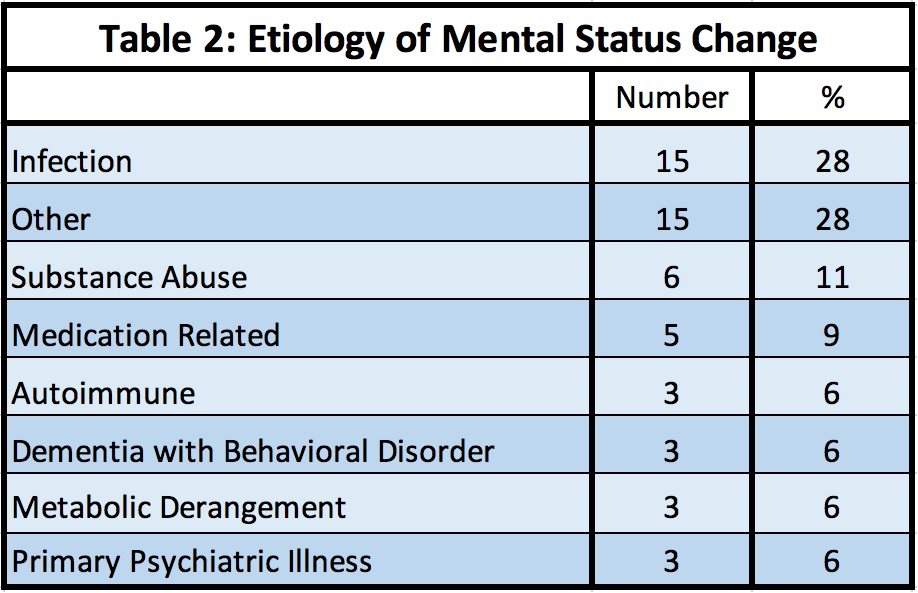
Methods: We performed a retrospective observational study of patients admitted to Parkland Memorial Hospital from September 1, 2018- September 30, 2019. We included patients with “altered mental status” or “delirium” or “confusional state” and any of the four lab components B12, folate, RPR and TSH. 862 patient records were retrieved, of which, to date, we have finished abstracting charts for 53 patients meeting eligibility criteria. We excluded deceased patients and patients who had the labs performed for reasons other than altered mental status. Data was collected on reason for admission, type of altered mental status (delirium, behavioral change, confusion, disorientation, psychosis, aggression, lethargy, suicidal ideation), documented etiology of altered mental status and actual values for the labs of interest in our study. We also abstracted pertinent co-morbidities and demographic information.The etiologies identified during the work up of AMS were categorized into infection, primary psychiatric illness, substance use disorder (including alcohol), dementia with behavioral disorder, metabolic derangement, autoimmune or other.
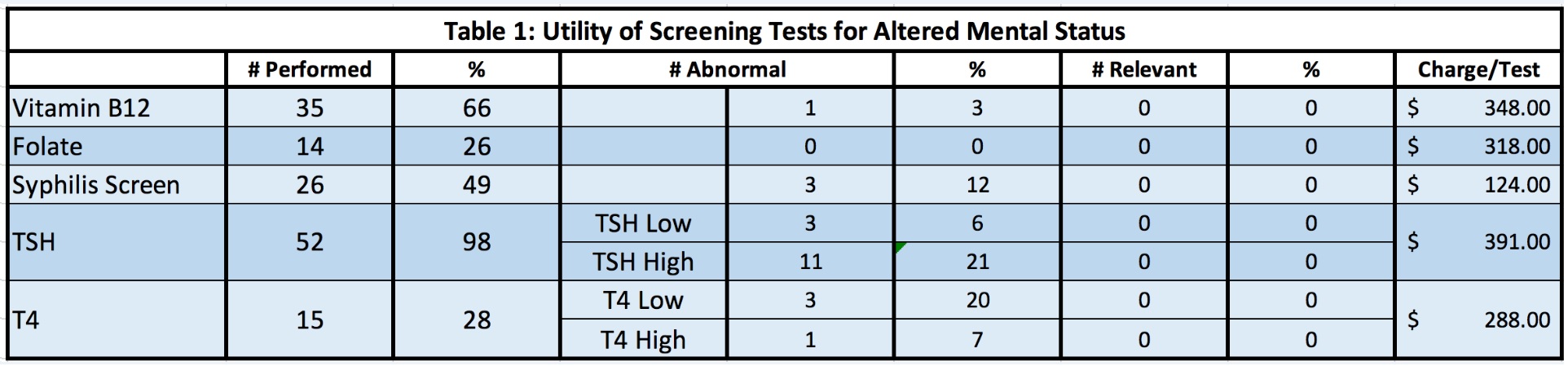
Results: Of the 53 patients who met our study criteria, there were 26 females (49.1%) and 25 patients (47.2%) were age 65+. The Black and Hispanic population constituted the majority at 19 patients and 21 patients, respectively. The breakdown of the labs showed that 35 patients (66%) had a B12 level checked, of which, 1(3%) had a low level. 14 patients had folate checked with no low values identified. TSH was done in 52 patients with 11 (21%) high TSH values. Of the 15 T4s that were checked, 1 (7%) was high and 3 (20%) were low (Table 1). 26 patients had an RPR checked; of which, 3 (12%) were abnormal.In the 53 cases reviewed, none of the results of B12, folate, TSH and RPR testing were ultimately related to the etiologies found for our patients’ AMS (Table 2). Charges for B12, folate, TSH, T4 and RPR testing on our 53 patients amounted to $44,508. Extrapolated to 862 patients, that would result in $723,885 in charges for our patients and, at a 30% cost/charge, $217,165 in non-value added, annual costs for our organization.
Conclusions: Altered mental status is common in hospitalized patients. Work up for altered mental status is reflexive and may not represent evidence based, high value care. Our preliminary results suggest that standardizing work-up for altered mental status in an evidence based, risk stratified, mindful and cost-effective manner could result in a substantial improvement in value for both our patients and health care organizations.