Background: Virtual Hospitalist (VH) care models are emerging in hospital medicine to address workforce shortages and improve patient access. VH programs are any programs where the hospitalist and patient are located at different sites, but the patient requires an acute level of care. This can include arrangements where: 1) the patient is located in a physical hospital, and the hospitalist is offsite (either at home or at another clinical location), 2) the patient is at home, and the hospitalist is located elsewhere (often called “Hospital at Home”), and 3) services can include admissions, discharges, and cross-coverage calls. Many single-site case studies have highlighted innovative programs such as virtual intake hospitalist(1) and hospital at home(2) programs, with many of these innovations catalyzed by the COVID-19 pandemic (3–5). Many of these programs are run by emergency medicine, general internal medicine, or geriatrics departments, therefore crosscutting perspectives of hospital medicine leaders driving adoption are poorly understood.Given the potential of VH programs to expand access, improve outcomes, and decrease costs, it is crucial to rigorously study and optimize these models. Key areas of focus include technical requirements, physician workflow, diagnostic accuracy, communication, and integration within the broader hospital system. With their rapid growth, VH programs are likely to play an integral role in the hospital of the future.
Methods: We conducted focus groups (FG) from a convenience sample of US academic hospitalist leaders participating in the Society of Hospital Medicine (SHM) Academic Leaders Special Interest Group (SIG) forum. Semi-structured interviews explored experiences with virtual hospitalist programs. Using rapid qualitative methods (6) including templated summaries and matrix analysis, audio recordings were analyzed using a blend of diffusion of innovation theory and social constructivism to identify key themes.
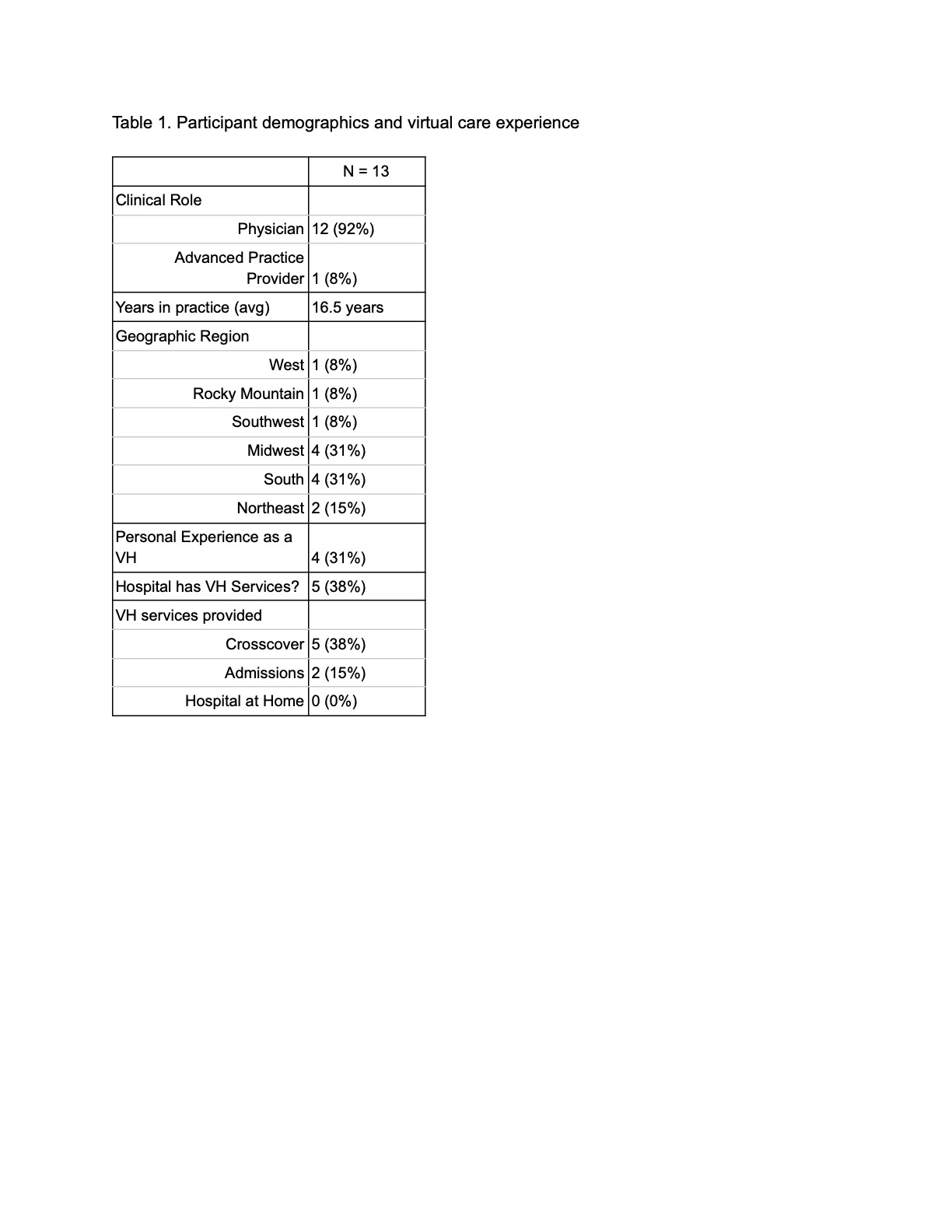
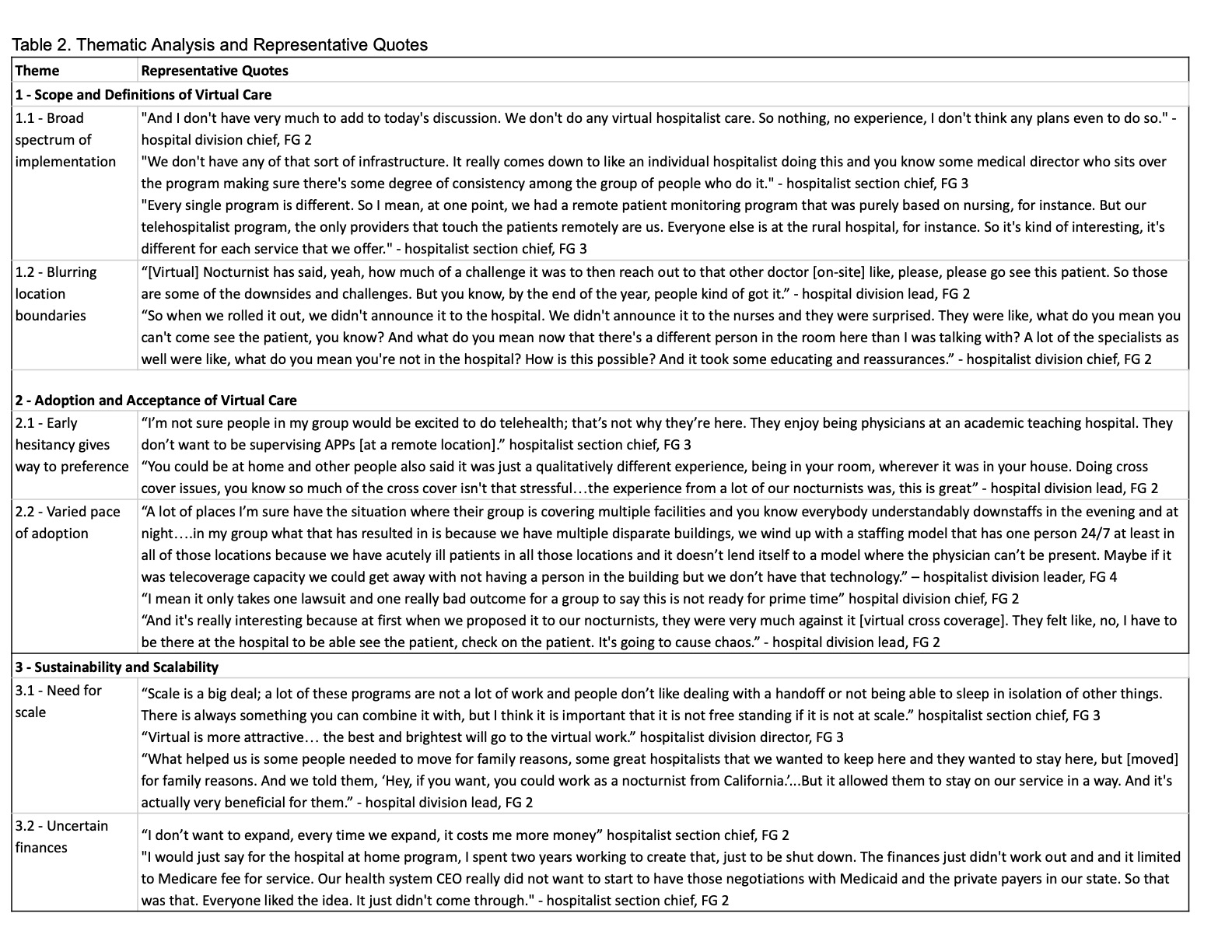
Results: We conducted four FG with 13 participants representing 9 hospital systems. Full demographics are in Table 1. Thematic analysis identified 3 primary domains: 1) Scope and definitions of virtual care varied widely, from basic phone cross-coverage to tele-admissions; 2) Adoption and acceptance of virtual care models followed a trajectory from hesitancy to preference as familiarity grew; 3) Sustainability and scalability of programs were threatened by unclear finances and need for a greater breadth of services. Representative quotes supporting these themes are highlighted in Table 2.
Conclusions: Hospitalist leader perspectives revealed complex factors influencing virtual care adoption and implementation. Addressing concerns about care quality, financing, and training may accelerate diffusion. Further research should clarify best practices for sustainable models optimized for both access and hospitalist experience.