Background: The Lumbar puncture (LP) success rate for graduating pediatric residents is around 54%, and residents often feel uncomfortable performing Lumbar punctures(LPs). An UALP(ultrasound-assisted lumbar Puncture) uses POCUS (point of care ultrasound) to visualize key anatomical landmarks for optimal and safe cerebral spinal fluid (CSF) collection. Evidence has shown improved LP success rates in pediatric and adult patients using the UALP approach. In addition, UALP has been shown to increase the confidence of emergency room providers in pediatric LPs.In contrast to emergency medicine providers, where ACGME mandates competency in POCUS, most pediatric residents currently have little or no formal ultrasound training. We hypothesized that teaching residents how to perform a UALP would improve their self-reported procedural self-efficacy in LPs.As POCUS continues to grow in popularity, our experience is timely for pediatric programs developing any POCUS curriculum because these insights are generalizable to other applications of POCUS.
Methods: In this Institutional Review Board-exempt mixed methods study, we implemented an educational innovation teaching pediatric residents UALP. The training consisted of three phases: First, online modules; Second, didactic sessions; Third, in-person workshop with hands-on practice and simulation. Of the 24 residents who participated in the course, 10 residents (42%) completed all the optional dependent measures to enable paired analyses.
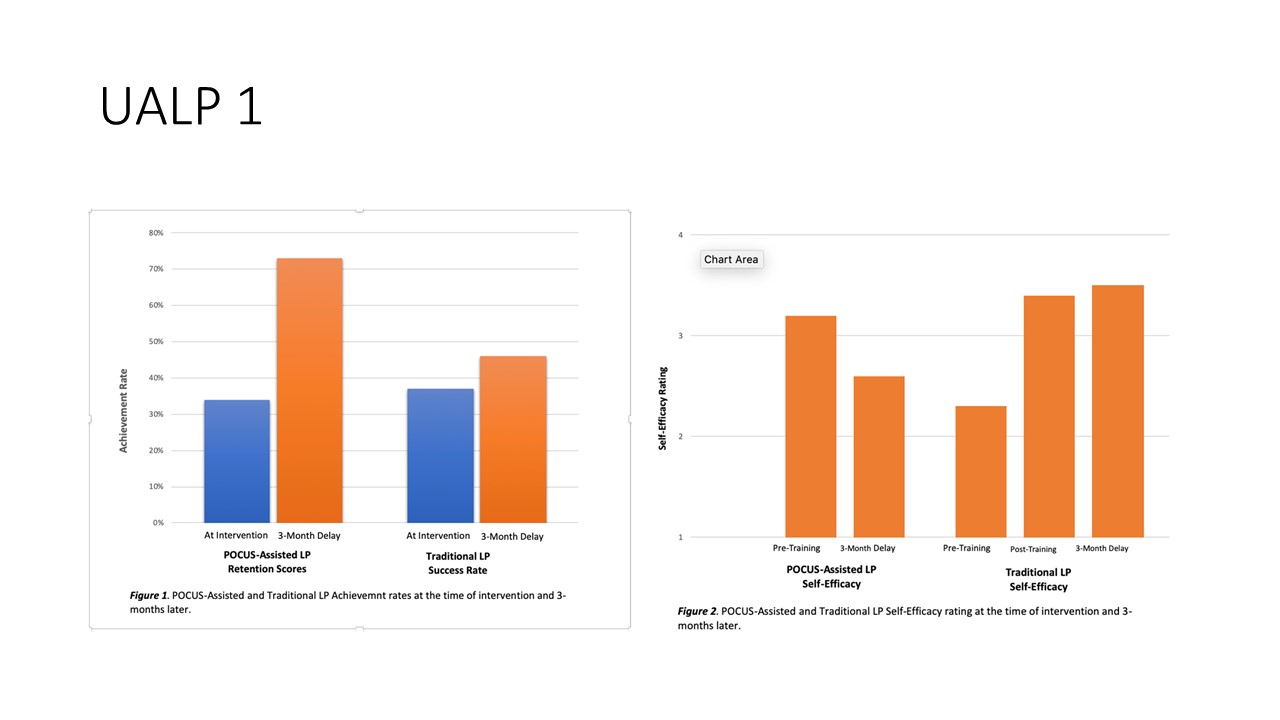
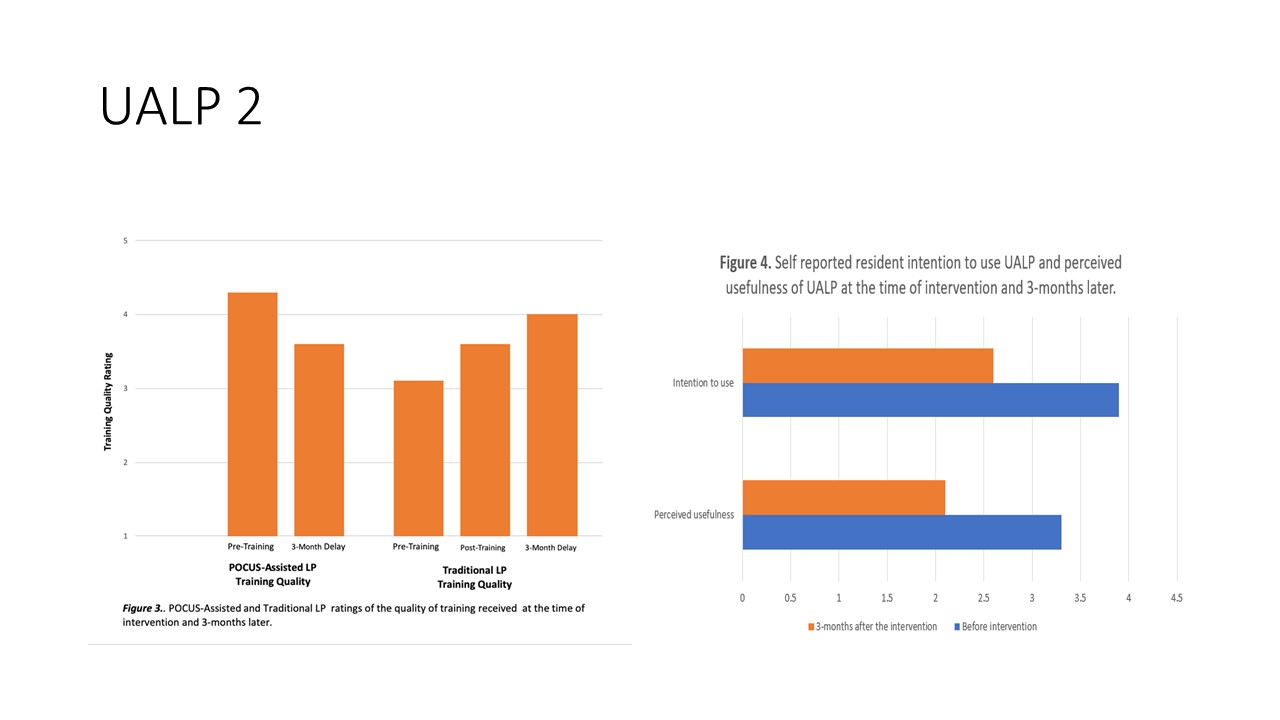
Results: Residents’ ability to identify and label landmarks increased from 34% at intervention to 72% 3 months later. Their self-estimates of LP success rate over a 3-month period also increased from 37% to 45%. Self-efficacy and technology acceptance with POCUS self-ratings decreased over a 3-month period; however, residents’ self-efficacy in performing LPs via the traditional method increased over time. Resident ratings of the quality of their education in performing LPs increased post-intervention; however, three months post-intervention, the ratings of the quality of their education in UALPs decreased. Three months post-training, the resident’s intention to use POCUS and perceived usefulness was significantly lower.
Conclusions: Although implementing our innovation in UALPs appeared to increase residents’ perceived ability to perform LPs, residents did not utilize their training in POCUS prior to performing LPs in clinical practice. Self-efficacy and technology acceptance with UALPs was high immediately post-intervention but decreased three months post-intervention.Future areas of research should include clarifying the role of UALP in pediatric hospital medicine and developing more validated tools for measuring provider competency in POCUS. We hypothesize that POCUS would have been utilized if our learners had ongoing training in clinical practice.