Background:
Improving patients’ readiness for discharge is an important aspect of care transitions. Eliciting barriers to discharge from patients and providing daily feedback to their physicians may provide an approach to identifying and addressing problems early in patient stays.
Methods:
We enrolled a random sample of patients admitted to the Medicine Service at a tertiary academic Medical Center. Patients were asked a 12-item Readiness for Hospital Discharge Survey covering functional status (pain, mobility, activities of daily living), knowledge (medications, problems to watch for), and coping ability (emotional support). We first surveyed patients within two days of admission and then followed them as frequently as possible until discharge. During the pre-intervention time period (11/2013-04/2014) data were collected but not given back to providers, after 04/2014 data were fed back to patient’s attending physician by daily email. We then compared barriers at discharge between time periods using t-tests and chi-squared tests. We also surveyed physicians who received the readiness for discharge information to assess use and clinical value.
Results:
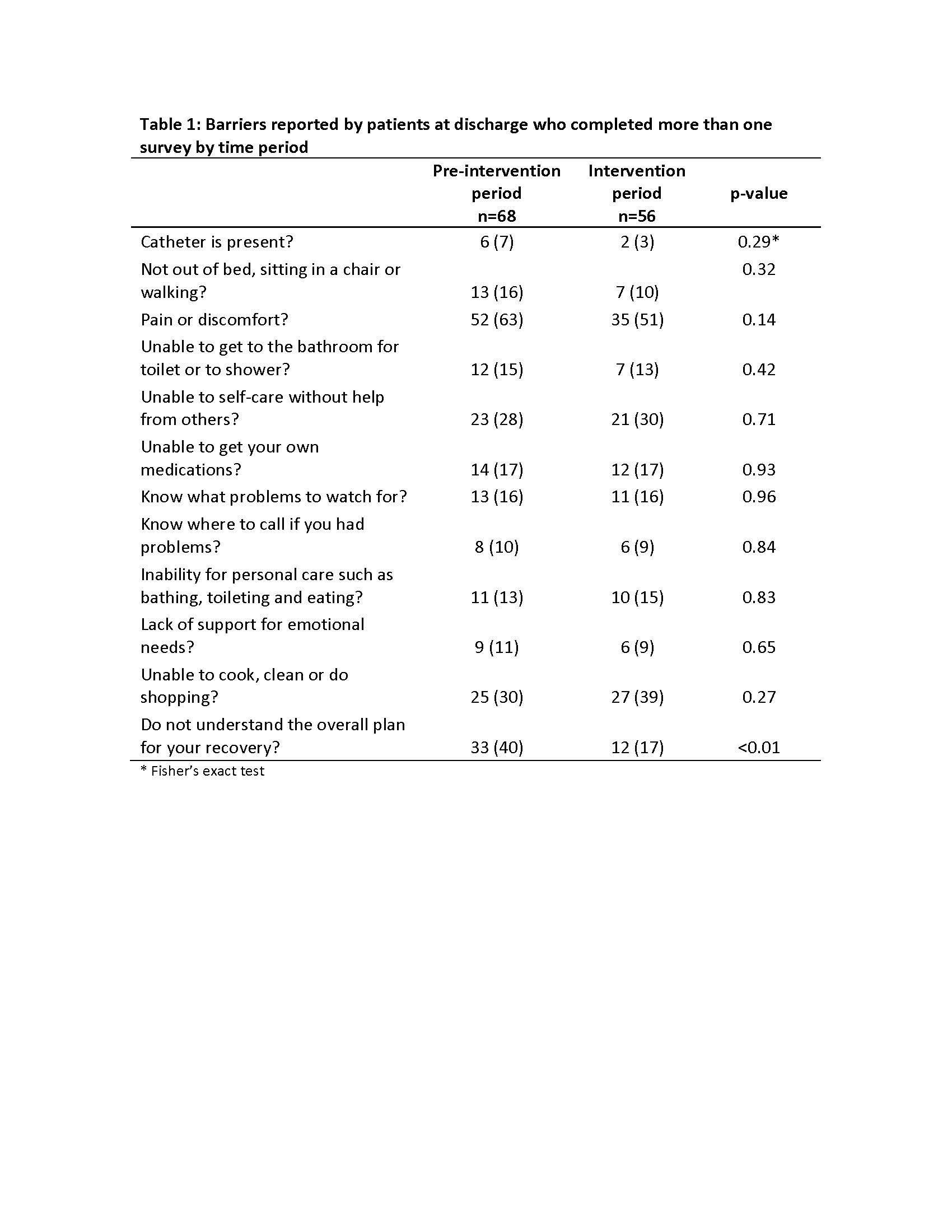
We enrolled 163 patients before feedback was given and 135 patients afterwards. Sixty-eight (42%) in the pre-intervention period and 56 (41%) in the intervention period completed at least two surveys. We did not observe a significant reduction in the mean number of barriers reported at discharge between the pre-intervention and intervention periods (2.53 versus 2.29; p=0.52). However, sixty-one patients (90%) in the pre-intervention period left the hospital with ≥1 persistent barriers compared to 42 (75%) of patients in the intervention period (p=0.03). While many specific physical barriers (such as activities of daily living, ability to self-care and pain) were unchanged, understanding of recovery plan (40% versus 17%; p<0.01) appeared to improve significantly (Table 1). Response rates for our physician survey were high (84%) but of the 65 respondents only 20 (31%) ‘strongly agreed’ or ‘agreed’ that the data was useful for planning discharge and 37 (56%) stated the data ‘rarely’ or ‘never’ highlighted anything new that the team was not already aware of.
Conclusions:
While feedback to physicians was not associated with changes in barriers to discharge based on physical problems, it was associated with better understanding of recovery plan and fewer patients with numerous barriers at discharge. Physicians’ survey data suggest areas of improvement in our feedback process, and may also represent challenges in terms of understanding how specific barriers might be addressed in hospitalized patients.