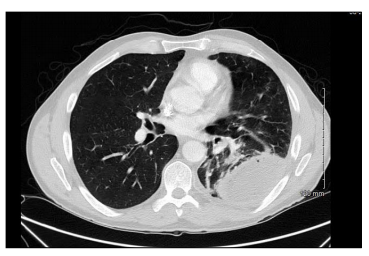
Case Presentation: 57 y/o Caucasian male with 45 pack year history and 6-weeks history of non-resolving community acquired pneumonia, treated with levofloxacin as an outpatient for 4 weeks, presents with 3 days of worsening cough, malodorous green sputum production, chills, subjective fevers and diaphoresis. He also reported a 20 pounds weight loss and poor appetite for 6 weeks. He was transferred from outside facility with leucocytosis at 18,000, with 81% neutrophils. Examination revealed diminished breath sounds on left base posteriorly. CT chest showed partially loculated large left pleural effusion with air consistent with left empyema. Patient was started on Zosyn and underwent left posterolateral thoracotomy with drainage of empyema, decortication and chest tube placement. Pleural fluid culture initially isolated Micromonas micros and gram-positive anaerobic bacillus. Antibiotics were changed to Ertapenem daily. Final cultures also grew Actinomycosis turicensis treated with penicillin G for 4 weeks followed by amoxicillin for at least 6 months.
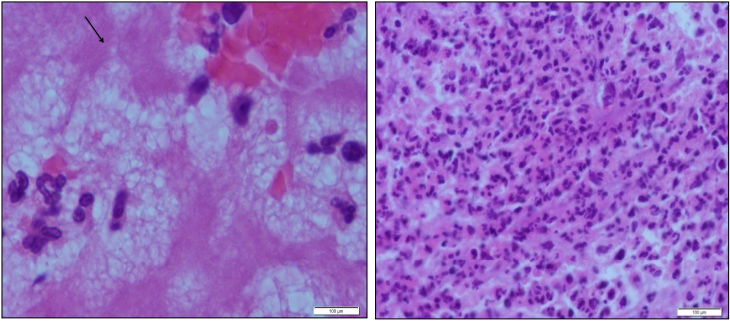
Discussion: Actinomycosis is an important cause of non-resolving pneumonia and this patient had persistent symptoms despite 4 weeks of appropriate antibiotic therapy. Pulmonary actinomycosis generally affects males in the 4th to 5th decade of life and often results from aspiration of oropharyngeal or gastrointestinal secretions. Poor oral hygiene and dental disease are known risk factors. This patient presented with the typical demographics and was observed to have several broken and decayed teeth. Micromonas is frequently associated with periodontal disease, indicating high possibility that poor dental condition was the likely source of infection. The patient also presented with common initial symptoms: chronic productive cough, fever and weight loss. Also, chronic tobacco use decreases mucosal defences and increases risk for actinomycosis infection. An approach to a non-resolving pneumonia would be a step wise assessment including: 1) repeat history for clues to unusual pathogens; 2) Chest CT and 3) bronchoscopy with bronchoalveolar lavage +/- transbronchial biopsy. The gold standard diagnostic test is tissue biopsy culture with anaerobic cultures. Unfortunately, the growth of Actinomyces is slow and can take up to 15–20 days before conclusion of a negative culture
Conclusions: Non-resolving pneumonia is presumed pneumonia that progress, resolve slowly, or fail to achieve complete resolution despite what is thought to be appropriate therapy. Hence, it is imperative that physicians can recognize the telling features and keep a high suspicion of pulmonary Actinomycosis when appropriate. Early, accurate diagnosis can prevent morbidity, including delayed diagnosis resulting in extended course of inappropriate antibiotics or unwarranted thoracic surgery due to complications.