Background:
Thoracentesis is a relatively safe procedure. Despite a lack of supporting evidence, common assumptions regarding safety guidelines include: (1) limit fluid removal to < 1.5 L; (2) avoid bilateral procedures; (3) do not tap patients on positive‐pressure ventilation (intubated or on Bi‐PAP); and (4) routinely obtain a postprocedure chest x‐ray. To assess the legitimacy of these assertions, we retrospectively analyzed a large volume of thoracentesis data generated by our Procedure Center at Cedars‐Sinai Medical Center.
Methods:
Five thousand consecutive thoracenteses performed over an 8½‐year period by a single operator at Cedars‐Sinai Medical Center were retrospectively analyzed. The primary outcome was the rate of major or minor procedural complications. Subanalyses were performed based on volume removed (1.5‐L cutoff), whether unilateral or bilateral procedures were performed, and whether or not the patient was receiving positive‐pressure ventilation (PPV) at the time of the procedure. Last, the frequency of postprocedure chest x‐rays was reviewed in relation to complications.
Results:
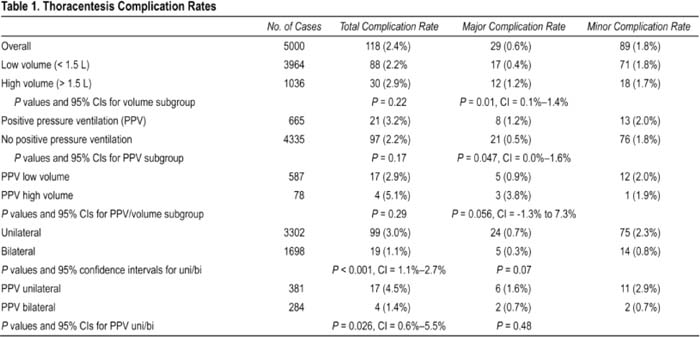
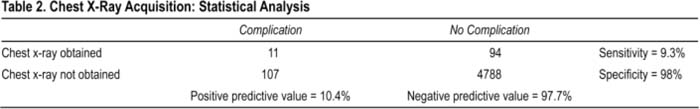
Table 1 breaks down overall, major and minor complication rates into 5 groupings. Major complications occurred at a significantly higher rate in the high‐volume and PPV groups. On the other hand, bilateral cases had a significantly lower overall complication rate than did unilateral cases. Table 2 displays the positive and negative predictive values, sensitivity, and specificity of chest x‐rays as they relate to postprocedural complications.
Conclusions:
Some widely held beliefs about safety parameters for thoracentesis do not appear to be supported by the evidence, whereas other teachings do have statistical validity. Overall complication rales in this series were lower than previously published rates. Within that context, there were significantly increased risks when removing high volumes (>1.5 L) and/or tapping patients on positive‐pressure ventilation. Surprisingly, patients who underwent bilateral thoracenteses had significantly fewer complications than did patients who had unilateral procedures. Further, our chest x‐ray data (although not comprehensive) strongly suggests that routine postprocedure chest x‐rays are not necessary. Ultimately, the decision about how much fluid to remove and whether to perform bilateral procedures, tap a patient receiving PPV, or obtain a chest x‐ray should remain in the purview of the treating physician. These decisions should be guided by an awareness of the evidence, individualized clinical assessments that take into account each patient's status (before, during, and after the procedure), and the operator's comfort. The risk of any procedure should be weighed against the potential clinical benefit so that clinicians can property advise patients and make informed decisions. Last, the importance of maintaining meticulous procedural data (both as individual practitioners and as group practices) cannot be overemphasized.
Author Disclosure:
M. Ault, none; B. Ault, none; B. Rosen, none.