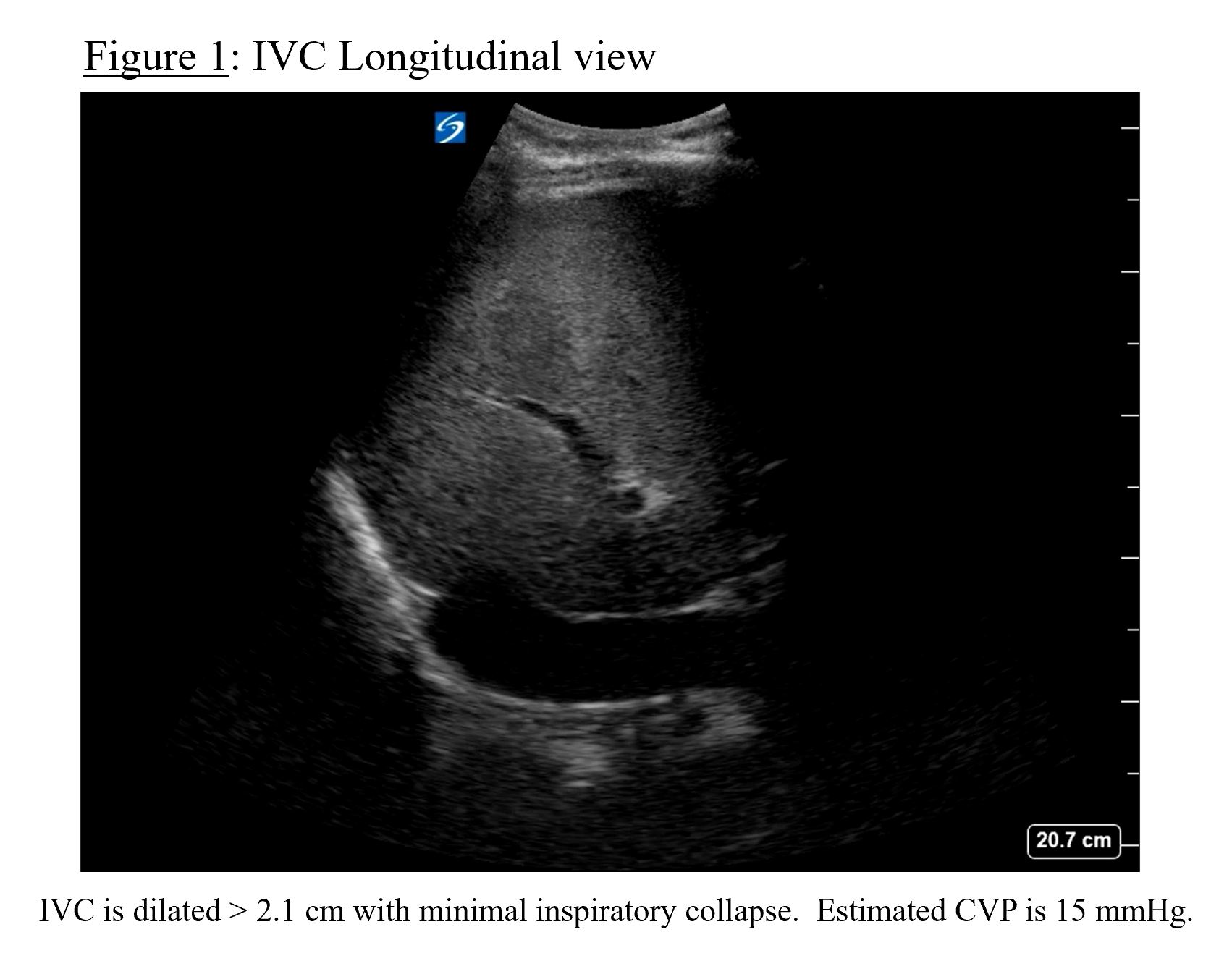
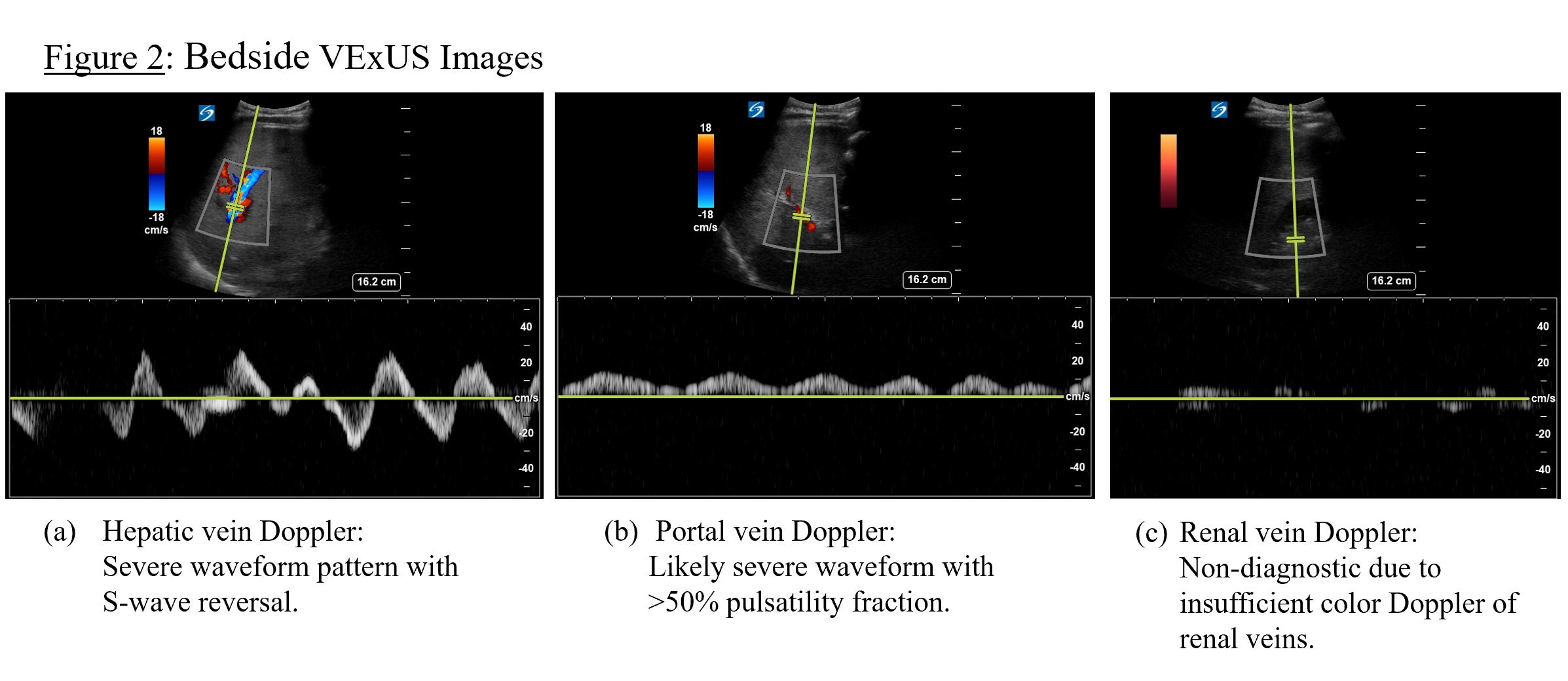
Case Presentation: A 73-year-old man with a past medical history of pancreatic adenosquamous carcinoma, biventricular heart failure with reduced ejection fraction (30-35%), and paroxysmal atrial fibrillation presented to the hospital with a 2-day history of bilateral lower extremity edema and 5-pound weight gain. Physical exam was notable for tachycardia, jugular venous distension, scleral icterus, and 3+ bilateral lower extremity edema. Labs were remarkable for BNP 2152 pg/mL, creatinine 1.4 mg/dL, INR 4.8, total bilirubin 5.3 mg/dL, alkaline phosphatase 280 U/L, AST 265 U/L, and ALT 184 U/L. The patient was admitted for acute decompensated heart failure with suspected congestive hepatopathy. Despite IV diuretics, liver enzymes worsened, and the patient developed hepatic encephalopathy with concerns for acute liver failure. CT abdomen/pelvis was remarkable for suspected passive congestion of the liver from right heart failure with overlapping steatosis and enlarging pancreatic tail mass (5.7 cm) without intraductal biliary dilation. Gastroenterology was consulted and obstructive etiology was ruled out. Workup for an infiltrative or autoimmune process was also negative. Although congestive hepatopathy was considered the most likely etiology, a transjugular liver biopsy for definitive diagnosis was recommended.Prior to biopsy, a Venous Excess Ultrasound Score (VExUS) using point-of-care ultrasound (POCUS) was obtained at the bedside and showed grade III severe congestion as evidenced by inferior vena cava (IVC) >2 cm (Figure 1), severe hepatic vein and likely severe portal vein Doppler patterns (Figure 2). Based on these findings supporting the diagnosis of congestive hepatopathy, a decision was made to escalate IV diuretics. Liver enzymes subsequently decreased, and gastroenterology no longer recommended a liver biopsy, saving the patient from an invasive procedure. Signs of acute liver failure resolved, and the patient was subsequently discharged.
Discussion: To our knowledge, this is the first documented case illustrating the use of POCUS as a diagnostic tool for congestive hepatopathy. Prompt diagnosis of congestive hepatopathy is crucial as this noninflammatory process is reversible and can mitigate the risk of irreversible cirrhosis and subsequent hepatocellular carcinoma if recognized early (1,2). Diagnosis is made with physical exam and laboratory tests; however, these are nonspecific, can be normal until advanced disease, and do not correlate with degree of fibrosis determined by biopsy (2).In the setting of acute liver failure and decompensated heart failure, a VExUS performed at the bedside could support the diagnosis of congestive hepatopathy and prevent the need for invasive procedures. After identification of a plethoric IVC, VExUS utilizes Doppler ultrasound to evaluate the hepatic, portal, and intrarenal veins (3). Based on venous waveform patterns (classified as normal/mild/severe), a VExUS categorizes the degree of organ congestion as normal, mild, moderate, or severe (3). In our case, recognition of severe congestion pattern with VExUS significantly altered diagnostic and therapeutic management with positive outcomes.
Conclusions: A VExUS obtained at the bedside helps support the diagnosis of congestive hepatopathy. Prompt diagnosis and escalation of diuretic therapy could significantly reduce morbidity and mortality. Further studies are needed to validate the use of VExUS in the diagnosis of congestive hepatopathy and evaluate patient outcomes.