Background: The 2001 Institute of Medicine Report Crossing the Quality Chasm cited a lack of care coordination as a contributing factor to the “chasm” between evidence-based and delivered care and suggests team-based models of care delivery. Hospitalists are tasked with increasing efficiency in inpatient care. LOS is designated as a measure of care coordination and efficiency. In fiscal year 2017, UAB Hospital implemented a version of interprofessional rounds called transition of care (ToC) rounds on all hospitalist units. ToC rounds clearly defines member roles with the overarching goal to ensure all care providers understand the “plan for the day and the plan for the stay”. We aimed to evaluate the potential impact of our distinct ToC round on LOS.
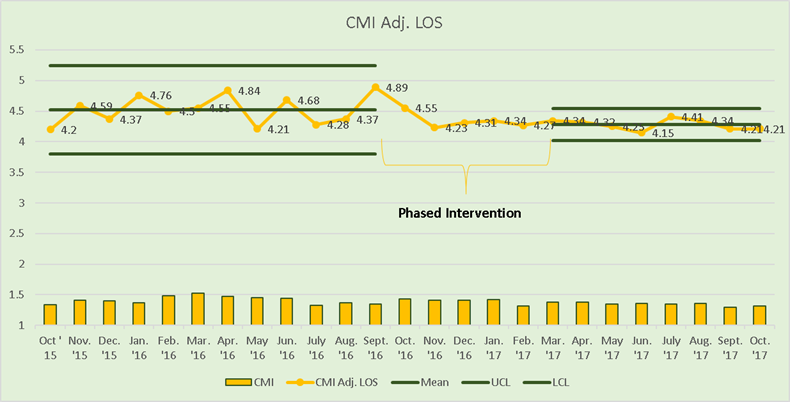
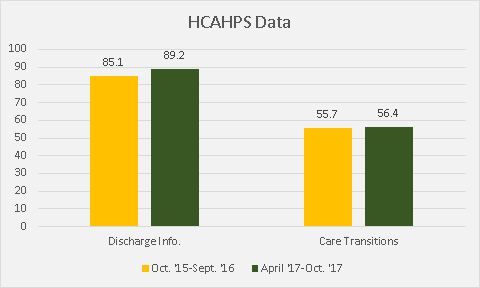
Purpose: ToC rounds were initiated sequentially on five hospitalist units from October 2016 through March 2017. ToC rounds includes hospitalists, bedside nurses, unit leaders, care transitions staff (case managers/social workers), with rehabilitation therapists and pharmacists attending most days. Each provider was trained in team goals, member roles, rounds structure/scripting, use of estimated date of discharge for proactive planning, use of whiteboards for communicating goals and discharge date to patients, and processes for addressing barriers to care progression. We analyzed LOS and Case-Mix Index (CMI) Adjusted LOS data for five hospitalist units, comparing all patients discharged pre- (10/2015–9/2016) vs post- (4/2017–10/ 2017) implementation of the new rounds. Secondary outcomes were discharge instructions and care transitions patient satisfaction scores on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.
Description: The hospitalist service discharged 6878 inpatients pre- and 4722 inpatients post-implementation of the ToC rounds from their five units. Of those discharges, 2830 (41%) pre- and 1996 (42%) post-intervention were Medicare patients. Mean LOS (6.09 +/- 8.5 vs 5.39+/- 5.9 days, P<.05) and CMI adjusted LOS (4.84 +/- 4.8 vs 4.23+/- 3.7 days, P<.05) for all patients were significantly reduced post-ToC rounds. Percent of patients reporting “strongly agree” on the HCAHPS survey significantly improved for discharge information (85.1% vs 89.2%, P=0.005) and showed no significant improvement for care transitions (55.7% vs 56.4%, P=0.77) between the pre and post-implementation periods.
Conclusions: Implementing daily ToC rounds with clearly defined member roles and team goals is feasible and improves care efficiency as measured by hospital LOS and patient satisfaction on discharge information.