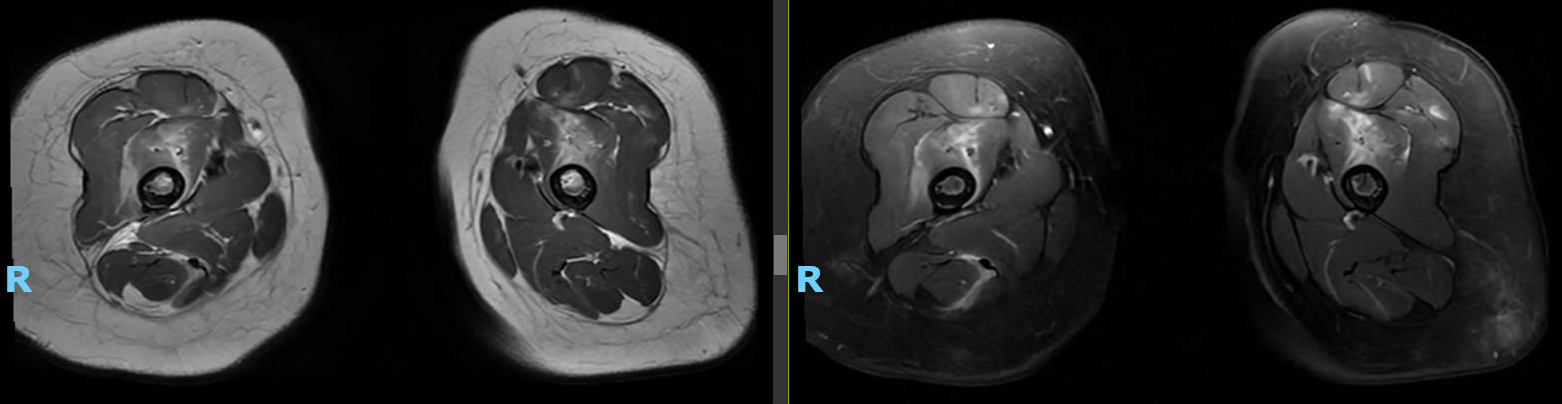
Case Presentation: A previously healthy 16-month-old girl presented to the emergency department with refusal to walk following a fall. She was lowering herself from a high bed when she fell backwards, hitting her buttocks and lower back without a head strike. Over the next couple days, the patient was fussy and less active. She refused to stand or walk and was eating less than normal. Prior to the fall, she had been meeting developmental milestones appropriately and walking without issue. The patient had rhinorrhea the week prior but no recent fever, cough, dyspnea, vomiting, diarrhea, abdominal pain, or rash. On exam she was afebrile with vitals within normal limits. She appeared uncomfortable with tender swelling of the midline lower thoracic region. She had full range of motion and appropriate strength of all extremities but cried with movement of the legs. Tone and reflexes were normal. When placed upright, her legs would stiffen and she would plantarflex before falling to a crouching position. Initial labs were notable for elevated ESR (57) and AST (102) with otherwise normal CBC, CMP, and CK. Radiographs of the thoracic spine, sacrum, and lower extremity were unremarkable as was total spine MRI. The patient was admitted for observation but showed minimal improvement despite administration of acetaminophen and ibuprofen. Given she was still far from baseline after a week, MRI of the brain and lower extremity were obtained which showed extensive inflammation of the pelvic girdle, thighs, and legs (see image).
Discussion: The differential diagnosis for this toddler with prolonged refusal to walk following a fall was initially broad, including trauma, infectious/inflammatory etiologies, neurologic disorders, toxic exposure, and hematological disease/malignancy. The failure of symptoms to improve prompted imaging revealing extensive muscle inflammation suggestive of an inflammatory (post-viral or autoimmune) vs. non-inflammatory myopathy. Further labs at this time were notable for continued normal CK and elevated AST with aldolase and LDH elevated (hemolyzed). An extended myositis panel revealed positive anti-MDA5 antibodies, and muscle biopsy confirmed diagnosis of juvenile dermatomyositis (JDM). JDM is a rare, autoimmune disease characterized by proximal muscle weakness and classic skin rashes but can affect multiple organ systems. Serologic testing may demonstrate elevated muscle enzymes and presence of myositis-specific/myositis-associated antibodies (1). Prevalence of anti-MDA5 antibodies in JDM patients varies based on ethnicity (7% in predominantly Caucasian cohorts vs. 38% in a Japanese cohort) and the associated clinical phenotype has been shown to include cutaneous lesions and interstitial lung disease with milder muscle disease and lower CK levels (2,3). Several aspects of this patient’s presentation were notable including the lack of characteristic skin lesions (e.g. Gottron’s papules, heliotrope rash, skin ulcerations) at the time of presentation as well as the young age at onset of symptoms (average onset of JDM is 7 years and anti-MDA5 antibodies have been associated with later onset of symptoms) (1,2).
Conclusions: This case highlights the need to consider a broad differential, including inflammatory conditions, in cases of sudden refusal to walk in pediatric patients. JDM is a rare inflammatory myopathy that can have diverse clinical presentation and should be considered even in very young patients without characteristic cutaneous findings.