Case Presentation:
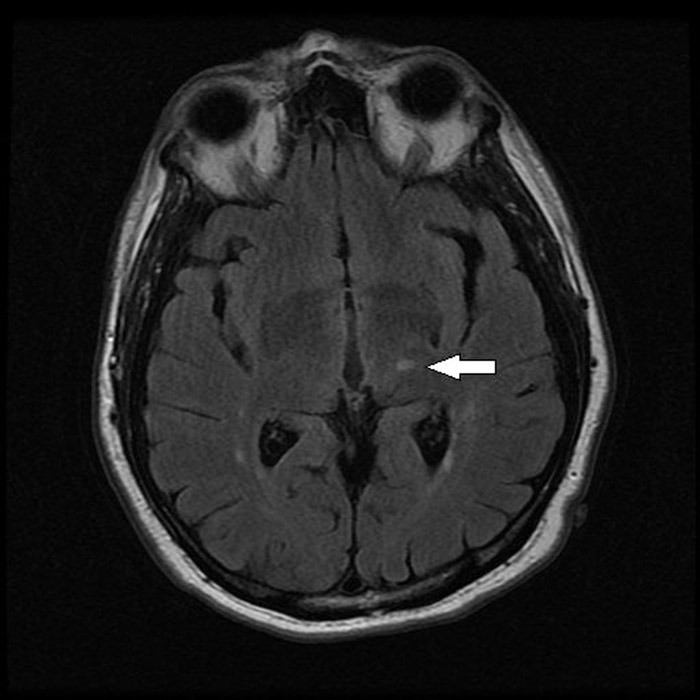
A 63‐year‐old right handed male with a history of hypertension, diabetes mellitus and active tobacco abuse presented with a five day history of right‐sided numbness and sharp pain in his left lower extremity for 1 day. On examination, he was alert, active and oriented to person, place, and time. His vital signs revealed marked elevation of blood pressure to 190/102 mmHg, pulse rate of 88 beats per minute (regular), and temperature 37.8°C. On neurological examination, he had hyperesthesia on the right side of the body demonstrated by exaggerated pain on light touch. No facial asymmetry or any motor deficits were noted. Babinski reflexes were bilaterally down going. CT scan of the head showed right‐sided old infarct in the corona radiata . Diffusion weighted magnetic resonance imaging (MRI) of the brain revealed sub‐acute infarcts in left corona radiata and punctate sub‐acute lacunar infarct in left thalamus (Fig 1 and 2). Echocardiogram showed no evidence of thrombus in the heart chambers or atrial fibrillation/flutter and Doppler imaging of the carotid artery was within normal limits. His right sided hyperesthesia was attributed to thalamic stroke syndrome. Gabapentin was started at 300 mg at bedtime and gradually advanced to 300 mg 3 times daily. His pain responded well to morphine initially which was later transitioned to tramadol. At 6 months’ follow up, his pain has been fairly well controlled with gabapentin and tramadol.
Discussion:
Thalamic pain syndrome is a rare condition, first described by Dejerine and Roussy in 1906, which develops after a thalamic stroke. It is one of the causes of central post‐stoke pain syndrome(CPSP) which occurs as a result of a vascular lesion of the ventro‐posterolateral nucleus of the thalamus .Though common after ischemic or hemorrhagic strokes involving the thalamus, CPSP can occur secondary to disruption of the somatosensory pathways of the brain at any level, i.e., thalamus, medulla or cerebral cortex. Diagnosis relies on a detailed history, accurate general and neurological examination, and imaging of the brain with the exclusion of other possible causes of pain.
Although not proven in clinical trials, combination therapy, as frequently used in clinical practice, may be effective. Amitriptyline and lamotrigine aimed at decreasing neuronal hyperexcitability, are considered first‐line. Opioids and lidocaine have been used with variable efficacy. Noninvasive stimulation therapy can be considered in refractory cases.
Conclusions:
CPSP remains a significant impediment in the lives of certain post‐stroke patients, with little in the way of effective treatment in the standard armamentarium, and further research is needed into novel treatments.
Caption: Fig. Axial T2 FLAIR MR image demonstrating subacute lesion with hyperintense signal in Lt. postero‐inferolateral region of thalamus (arrow)