Background:
Increasing the value of health care, typically regarded as maximizing quality of care while minimizing unnecessary costs, has been an increasing focus of hospitals nationwide. Ways of reliably measuring unnecessary utilization, however, have not been well-studied.
Hospital Compare is a consumer-oriented CMS.gov website that provides information on how well hospitals provide evidence-based care. It displays quality statistics in various domains, including rates of unnecessary medical imaging. One such measure is the use of cardiac stress imaging prior to low-risk procedures, which is costly and not recommended by multiple professional guidelines, including those published by the American College of Cardiology/American Heart Association and the American Society of Anesthesiologists. According to Hospital Compare, our institution orders such unnecessary testing at a rate substantially higher than the national average (8.6% versus 5.3%). We sought to understand the reasons behind this alarmingly high rate, and whether it was truly reflective of unnecessary procedures.
Methods:
We conducted a single-center retrospective chart review of all patients who underwent a cardiac stress imaging procedure within 30 days prior to a low-risk procedure from July 2014-July 2015, as defined by the CMS measure. Cases were included if both the cardiac stress imaging exam and low-risk procedure were performed at NYU; there were no exclusion criteria. We examined whether the stress imaging procedure was ordered exclusively for pre-operative workup for a low-risk procedure, or whether it was ordered for an alternative clinical reason.
Results:
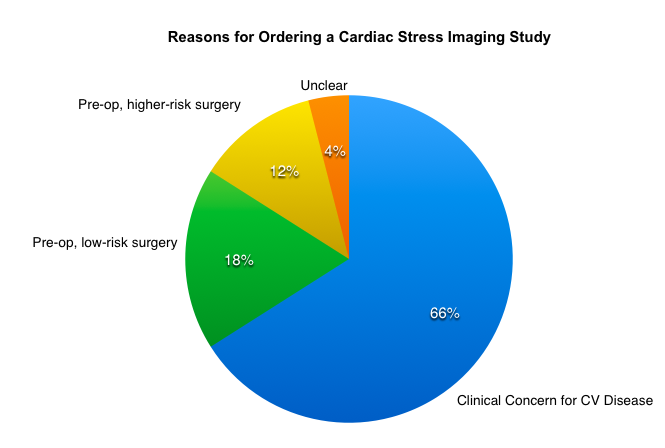
Over a one year period, 168 cases met inclusion criteria. A total of 109 (66%) of the cardiac stress imagine procedures were ordered for a clinical presentation concerning for underlying cardiovascular disease and were independent of the pre-operative evaluation. 30 (18%) were ordered expressly for pre-operative workup in anticipation of a low risk procedure, 21 (12%) were ordered for pre-operative evaluation prior to a high-risk procedure, and 7 (4%) were ordered for unclear reasons. The higher-risk procedures were primarily solid organ transplants, for which the pre-procedure evaluation also included a low-risk procedure (eg, colonoscopy). Of the 30 cardiac stress imaging procedures ordered solely for pre-operative workup, the most common anticipated low-risk procedure was endoscopy, including colonoscopy and upper endoscopy.
Conclusions:
Our study demonstrated that the vast majority of cardiac stress imaging procedures assumed to be pre-operative in nature as reported by Hospital Compare were actually ordered for another, likely valid, clinical indication. These results suggest that the Hospital Compare method is a sub-optimal measure of unnecessary imaging and perhaps quality overall. Opportunities for institutional improvement exist, however, in minimizing cardiac stress imaging prior to endoscopic procedures.