Background: Patient out-of-pocket costs are a critical consideration when providing care as they can represent a substantial portion of a patient’s income and when they are exceedingly high can become a barrier to care. We sought to better understand Physician interaction with and reaction to out-of-pocket costs at the trainee level.
Methods: A nineteen-question survey was sent to all Internal Medicine Residents at our institution, a three-hospital, academic residency program involving a Veteran’s Affairs hospital, a tertiary referral hospital, and a safety-net hospital. Residents rotate on inpatient and outpatient services at all three sites and have a primary care clinic at the county hospital or the Veteran’s Affairs hospital. The survey was sent at the end of the academic year. Participants were asked to answer general questions as well as questions related to their most recent panel of inpatients and their clinic patient panel.
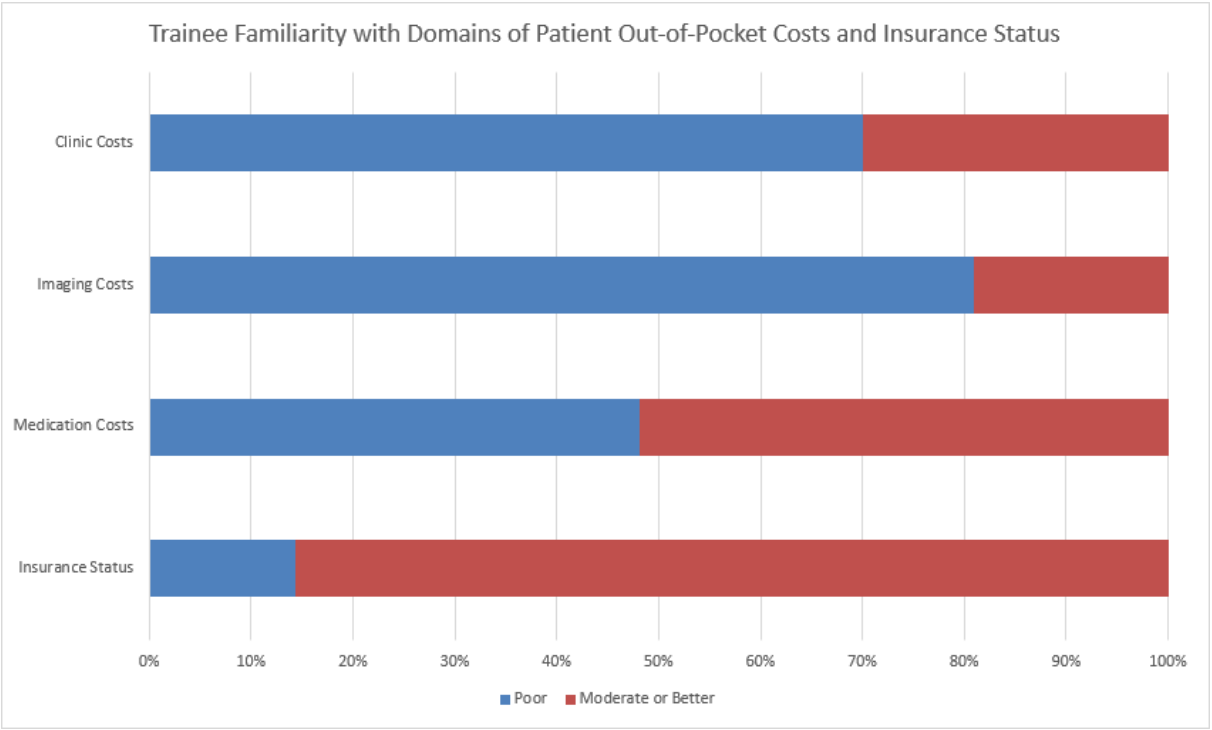
Results: Out of 159 residents 106 (67%) responded, with similar response rates from first- and second-year trainees with a lower response rate from third-year trainees (70%, 71%, and 59%). Familiarity with patient insurance status and costs associated with medications was the highest (85% and 52% moderate or greater, respectively), with costs associated with imaging and clinic visits lower (19% and 30% moderate or greater, respectively). There was no significant difference in responses by clinic site. There was a significant difference when respondents were asked to consider outpatients compared to inpatients, with significantly higher familiarity attributed to clinic patients’ out of pocket costs when considered associated with clinic visits, imaging tests, and medications. When answers were compared between years of training, no significant difference was seen in any responses given.
Conclusions: Our survey demonstrates that trainee self-reported familiarity with various patient out-of-pocket costs was low and was not significantly affected by year of training. Results were significantly positively affected when considering a patient in the clinic as compared to an inpatient. This suggests that there is a gap in trainee knowledge around these topics. A lack of improvement across levels of training suggests that trainees learn all they can meaningfully incorporate by the end of their first year of training and that exposure to individual patient cases does not directly correlate to increased familiarity with out-of-pocket costs. A lack of difference corresponding to respondent’s clinic site may reflect the similarity between coverage in the Veteran’s Affairs system and in our county hospital, where almost all clinic patients are eligible for near-total financial assistance. A difference in attitudes comparing inpatient to outpatient site of care may reflect the longitudinal clinical experience trainees have with patients in the clinic or the relative heterogeneity of admitted patients. Developing familiarity with out of pocket costs during training can likely make practicing physicians more aware of the financial realities of their patients, enabling them to provide the best care. How to achieve this knowledge and incorporate its use into the numerous other responsibilities in a given patient encounter remains an open question.