Background: Several case reports and case series have found that transcatheter mitral valve procedures (TMVP) improve hemodynamics and reduce symptoms in patients with mitral valve disease and concomitant hypertrophic obstructive cardiomyopathy (HOCM).(1-6) There is a lack of evidence regarding the outcomes of patients that undergo TMVP with HOCM, however several studies have evaluated the outcomes of transcatheter aortic valve replacement (TAVR) in patients with HOCM.(7-9) These studies have shown a higher incidence of in hospital mortality, net adverse cardiovascular events, acute kidney injury (AKI) and hemodialysis, vascular complications, permanent pacemaker requirement, aortic dissection, cardiogenic shock, and mechanical ventilation requirement.(7-9) The present study examined a large nationally representative cohort to evaluate clinical outcomes of patients with HOCM after TMVP.
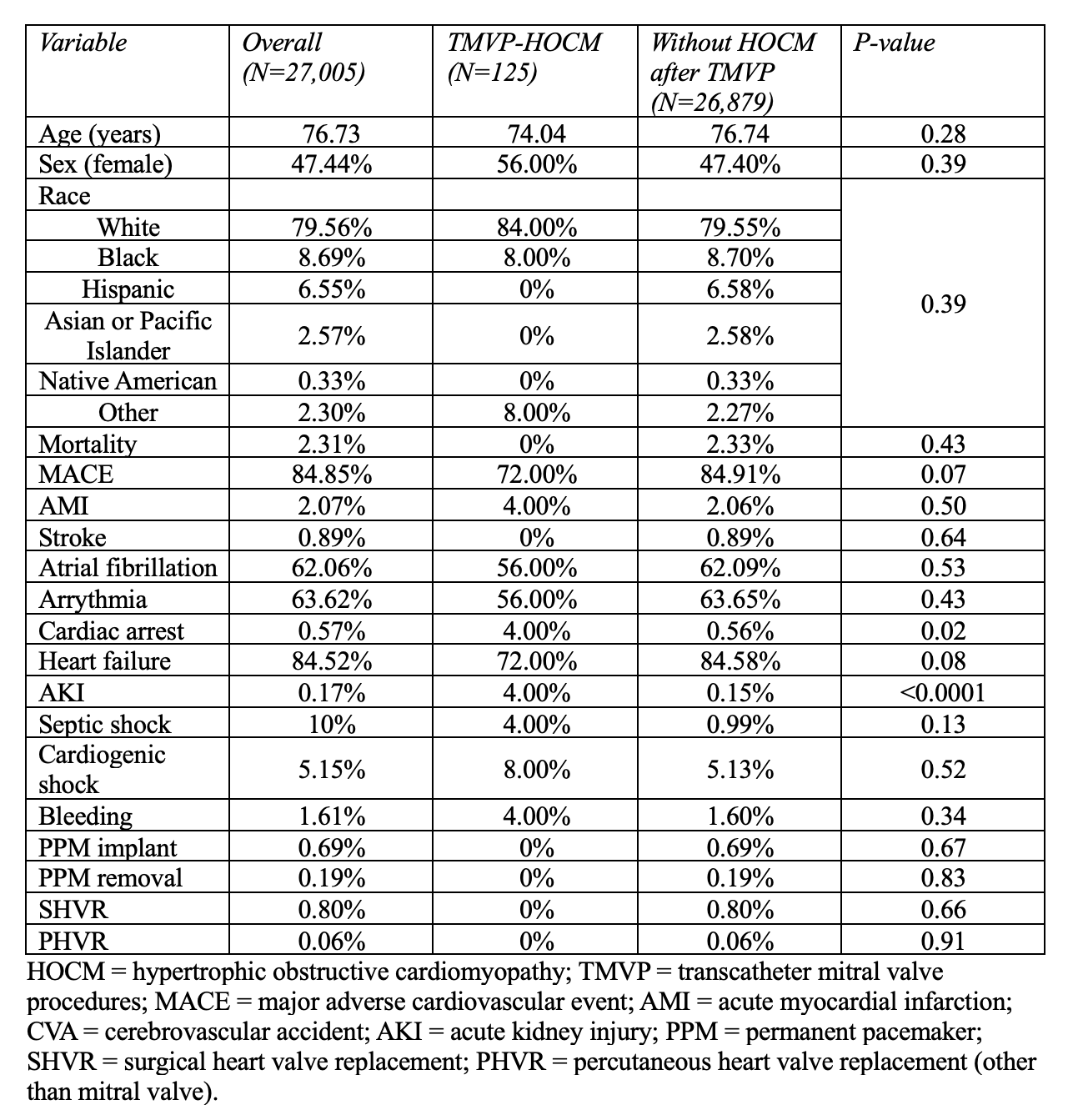
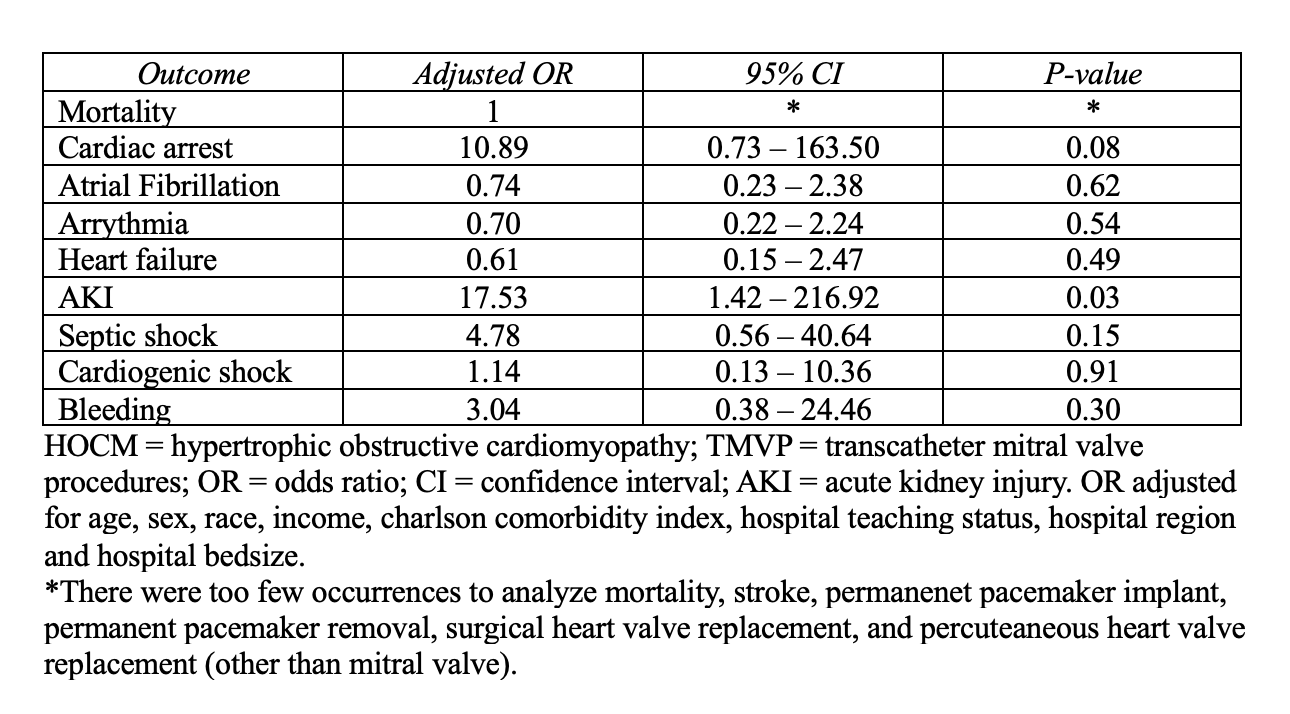
Methods: Patients (age ≥ 18 years) from the National Inpatient Sample database who underwent transcatheter mitral valve repair and replacement between January 2017 to December 2019 were selected and a retrospective, cross-sectional design was utilized. Pearson chi-squared analysis was used to compare prevalence of characteristics listed in Table 1. Outcomes of those with and without HOCM that underwent TMVP were analyzed using multivariate logistic regression adjusted for age, sex, race, income, charlson comorbidity index, hospital teaching status, hospital region and hospital bedsize. For both analyses, p-values of less than 0.05 were considered significant.
Results: We identified 27,005 patients who underwent TMVP during the study period, and 125 (0.46%) had concomitant HOCM. Demographic characteristics were similar in patients that had a TMVP with HOCM vs without HOCM (Table 1). There was a significant difference in the rates of AKI (4.00% vs 0.15%, p < 0.0001) and cardiac arrest (4.00% vs 0.56%, p=0.02) in patients with HOCM vs those without HOCM, respectively. There were no significant differences in rates of in-hospital mortality (0.00% vs 2.33%, p = 0.43), stroke (0.00% vs 0.89%, p = 0.64), cardiogenic shock (8.00% vs 5.13%, p = 0.52) or bleeding (4.00% vs 1.60%, p = 0.34) in patients with HOCM vs without HOCM, respectively (Table 1). Patients with HOCM had higher adjusted odds of acute kidney injury (AKI) (OR 17.53, 95% CI 1.42 – 216, p = 0.03) (Table 2).
Conclusions: Patients who underwent TMVP with concomitant HOCM had similar rates of in-hospital mortality, stroke, cardiogenic shock and bleeding as patients without HOCM, however there was a higher rate of AKI after TMVP in patients with HOCM. We only identified one other large study in the literature on TMVP patients with HOCM, which utilized the national readmission database.(10) This study found that patients with HOCM had higher odds of in-hospital mortality, stroke, and length of stay compared to those without HOCM that underwent MitraClip, and presence of AKI was not statistically significant between patients with HOCM (22%) and without HOCM (15%),(10) which does not align with our results. Further research in this population is needed to understand prognostic significance and to prevent AKI occurrence in patients undergoing TMVP.