Background: The use of physical restraints (PR) in the hospitals among patients is associated with increased delirium, pressure ulcers, prolonged ventilator use, post traumatic stress disorder and disruption of therapeutic relationship with the healthcare team. The current scientific research suggests their ineffectiveness for patient safety like preventing falls or dislodging medical devices. There has been a call to reduce the use of PRs in the hospital by multiple governmental and professional medical societies. We conducted this study to examine the change in rates of PR use and associated outcomes among hospitalized adults between 2011 to 2019.
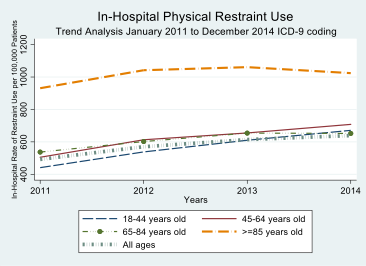
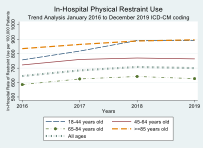
Methods: We used National Inpatient Sample databases to determine trends of PR usage among adult patients admitted to the hospital in the US from 2011 to 2019. Restraint use was identified using corresponding ICD-9 (during 2011-2014) and ICD-10 (during 2015-2019) code. We also compared years 2011-2012 and 2018-2019 to compare in-hospital mortality, length of stay, and total hospital charges.
Results: Of the 242,994,110 hospitalizations during the study period, about 1,538,791 (0.63%) had the use of PRs. There was a significant increase in PR use from 2011-2014 (p-trend< 0.01), although the overall rate remained stable from 2016-2019 (p-trend=0.07). There was variability in the trends of PR use by age groups. The restraint use increased in all age groups from 2011 to 2014 except for those above 85 years. The PR use remained stable in all age groups from 2015-2010 except for those between 18-44 years. Patients with PR had higher adjusted odds for in-hospital mortality in both 2011-2012 (adjusted Odds Ratio {aOR}=3.9 [CI: 3.7-4.2]; p< 0.01) as well as 2018-2019 (aOR = 3.5 [3.4-3.7]; p< 0.01). There was higher resource utilization among patient requiring restraints in the hospital with prolonged length of stay in 2011-2012 (adjusted Mean Difference {aMD}=4.3 days [CI: 4.1-4.5]; p< 0.01) and even longer in 2018-2019 (aMD=5.8 days [5.6-6.0]; p< 0.01). Total inflation adjusted hospital charges were higher for patients with PR in 2011-2012 (aMD= +$55,003 [CI: $49,309 - $60,679]; p< 0.01) and 2018-19 (aMD= +$70,018 [CI: $65,355 - $74,680]; p< 0.01.
Conclusions: Our study highlights the use of PR has remained high in the US hospitals despite the efforts to decrease their use. The data suggests a need to advance efforts for evidence-based strategies and implementation science to reduce PR use.