Background: Central venous lines (CVL), including temporary dialysis catheters, are often required in the inpatient setting. While CVLs are frequently placed in radiology suites or intensive care units (ICU), many institutions allow placement on medical-surgical wards by Hospitalist Bedside Procedure Services (BPS). The BPS at our institution began to perform CVL placement at the patient bedside on medical-surgical wards in 2015 and also placed CVLs for many transplant ICU patients during daytime hours from 2015-2017 until the transplant ICU hired a dedicated intensivist team and the BPS transitioned almost exclusively to ward patients. Our goal was to compare the patient risk profiles of CVLs placed in the ICU to medical-surgical wards and outcomes in terms of complications and unsuccessful attempts in the two settings.
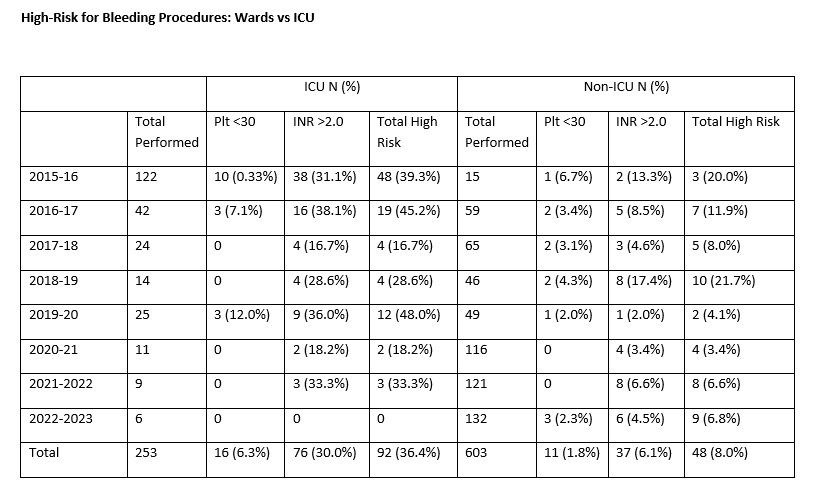
Methods: The Hospitalist BPS at our institution began to perform CVL placement at the patient bedside on medical-surgical wards in 2015. Patients were monitored via a portable cardiac monitor system during the procedure. All CVL placements were done under direct ultrasound guidance by attendings on the BPS or resident physicians with attending guidance. We evaluated internally collected data from the procedures performed by the BPS from 2015-2023 including complications and unsuccessful attempts as well as coagulation parameters. Patients were defined as high-risk for bleeding if platelets were < 30,000/µL or International Normalized Ratio (INR) was >2.0.
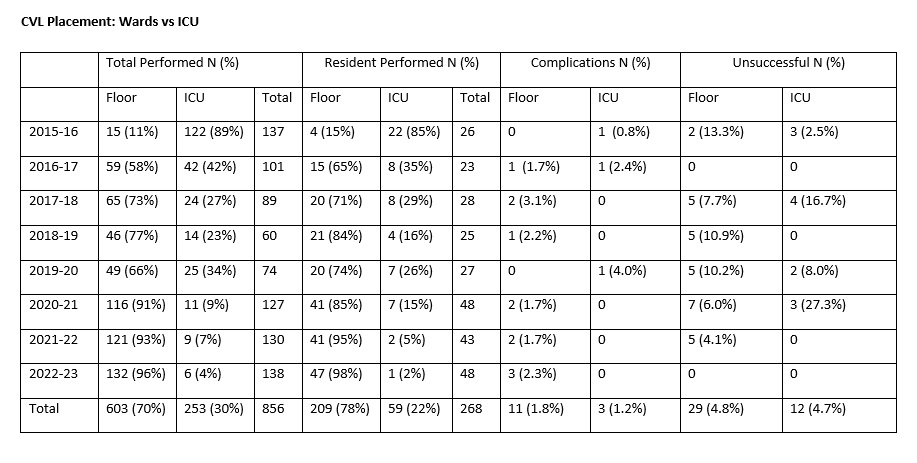
Results: The distribution of CVL placement shifted from 89% done in the ICU in academic year 2015-16 to 96% done on non-ICU patients in 2022-23. A total of 603 were done in non-ICU patients and 253 in ICU patients from 2015-23. The ICU had a significantly greater number of high-risk for bleeding patients compared to the non-ICU patients (36.4% vs 8.0%, p< 0.0001). There was no significant difference between placement on the wards and in the ICU for either complication rate (1.8% vs 1.2%) or rate of unsuccessful procedure (4.8% vs 4.7%). There was also no difference in the average number of needle passes between ICU and non-ICU patients (1.15 vs 1.2). Learners assisted with significantly fewer CVLs in the ICU compared to the wards (22% vs 78%, p=0.002).
Conclusions: The unique situation of transitioning from doing CVLs predominantly in ICU patients to almost exclusively non-ICU patients from 2015-2023 allowed for a fairly direct comparison in risk and outcome profiles. As expected, the ICU patients were at a significantly higher risk for bleeding at the time of CVL placement. Despite a higher risk profile, there was no significant difference for either complication rate or rate of unsuccessful procedure. CVL placement did not appear to be more technically difficult in ICU patients as the average number of needle passes was similar, but staff proceduralists appeared to be less comfortable with allowing learners to participate in ICU CVL placement.