Background:
Discharge from the hospital is a critical transition point in a patient's hospitalization. Poor hand‐offs at discharge can lead to adverse events for the individual patient, and result in avoidable re‐hospitalizations. Care transitions are especially important for elderly and other high risk patients who have multiple co‐morbidities. Standardizing the elements within the discharge process is the first step in addressing the quality and safety gaps evident in the transition from the hospital to outpatient setting.
Methods:
The Society of Hospital Medicine's Hospital Quality and Patient Safety committee assembled a panel of care transition researchers, process improvement experts and hospitalists to review the literature and develop an ideal discharge checklist for adult patients. The discharge checklist was presented at the Society of Hospital Medicine's Annual meeting in April 2005 and reviewed and revised by over 120 practicing hospitalists and hospital‐based nurses, case managers and pharmacists.
Summary of Results:
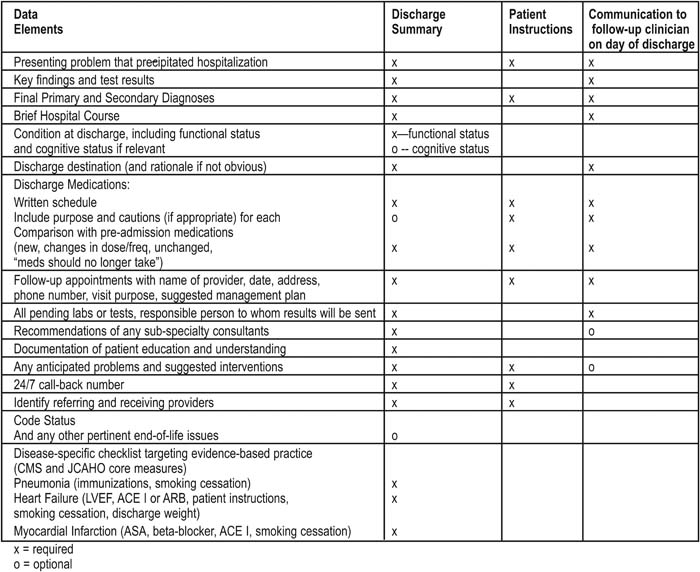
We present the finalized checklist in the accompanying table which includes a comprehensive list of the content necessary to optimize the discharge hand‐off, focusing on medication safety, patient education and follow‐up.
Statement of Conclusions:
The development of content standards for the discharge transition is the first step in improving the care hand‐off from the inpatient to the outpatient setting.
Ideal Discharge for the Elderly Patient: A Hospitalist checklist
Data Elements and Processes
Comments on Selected Checklist Items
Discharge summary – written with receiving caregiver in mind
Condition at discharge – Cognitive assessment: rather than a Folstein score, consider some description mention of mental capacity such as:
Lucid (full capacity for understanding and executive function, such as being able to follow instructions)
Forgetful (some senescence or impairment of memory)
Dementia (or “Brain Failure” ‐ incapable of reliable recall and/or executive function)
Discharge Medications
Medication reconciliation: discharge medications must be reconciled with preadmission medications
Consider NO TEARS Tool for medication review
Indications of medications required for Continuing Care (Nursing Home, etc.)
Consider clinical pharmacist involvement (especially if cognitive impairment, or ≥ 3 Medication changes)
Follow‐up for Hazardous Medications: 4 plans for proximate follow‐up (about one week) for tests and/or visits for patients taking (new or changed):
Warfarin
Electrolyte‐disturbing medications (diuretics)
CV drugs
Corticosteroids, or Hypoglycemic agents
Narcotic analgesics
Follow‐up appointments
2 weeks generally
Sooner if fragile clinical condition
Patient Instructions
Provide written instructions at 6th grade level
Teach‐back to confirm patient understanding
Code Status: Include at the least one of the following designations:
Full code (unrestricted full therapy)
DNR (Do not resuscitate)
Hospice‐type care, or “Comfort measures only”
Author Disclosure Block:
L. Halasyamani, Chair Hospital Quality and Patient Safety Committee Non‐remunerative positions of influence; D. Manning, None; S. Kripalani, None; T. Bookwalter, None; E. Coleman, None; J. Nagamine, None; J. Schnipper, None; P. Torcson, None; C. van Walraven, None; T. Budnitz, Society of Hospital Medicine Employment (full or part‐time).