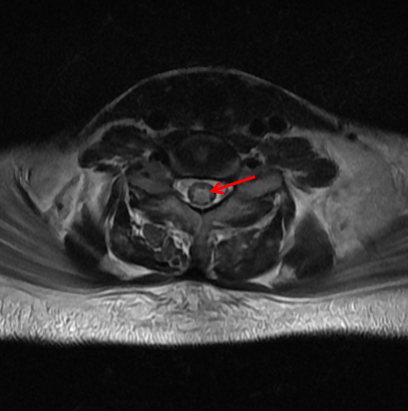
Case Presentation: A 25-year-old female patient presented to the hospital with intermittent fever and frontal headache for the past month and sudden onset bilateral lower limb sensorimotor weakness along with sphincter dysfunction for the past 2 days. There was no history of neck rigidity or back pain. No incidence of trauma, dizziness, or loss of consciousness was noted. The patient was diagnosed with Rheumatoid Arthritis 2 years ago and has been on glucocorticoid therapy ever since. On presentation, the vital signs were normal. Neurological examination revealed the absence of muscle tone (0/5) and power(0/5) in the lower limbs. The knee, ankle and plantar reflexes were absent along with decreased sensations of pain, touch and proprioception in the lower limbs. Laboratory tests revealed low complement (C3, C4) levels and positive Antinuclear antibodies (1:80) with a speckled nucleolar pattern. We found antibodies against dsDNA, nucleosome, Sm/RNP and SSA/Ro nucleoproteins, on further antibody profiling. Serum Aquaporin-4 (AQP4) receptor antibody and Myelin oligodendrocyte glycoprotein (MOG) antibody assay were negative. No oligoclonal bands were found in CSF. MRI spine showed T2-weighted hyperintensities from the T2 vertebra to the conus medullaris and in the medulla oblongata. Post-gadolinium enhancement was absent. (Fig.1, Fig.2) The patient failed to respond to the 5-day course of intravenous Methylprednisolone. Following this, 5 cycles of Plasmapheresis were carried out. Since no clinical improvement was seen, the Cyclophosphamide regimen was initiated. A few days later, the patient died as a result of severe acute respiratory distress syndrome.
Discussion: Transverse myelitis (TM) is one of the least but potentially severe complications of Systemic lupus erythematosus (SLE) and affects around 1-2% of patients with SLE. (1) It causes sensory, motor, and autonomic nervous system dysfunction, and leads to extensive and severe neuropsychiatric symptoms. (2,3) Clinical manifestations of TM arise from immune-mediated parenchymal damage with interruptions in the descending and ascending spinal tracts causing significant morbidity and mortality. (4) Based on the involvement of the nervous system, TM can be classified into Grey matter myelitis and White matter myelitis. (5) Grey matter myelitis is an acute condition characterized by flaccid paralysis and a well-defined sensory level, whereas white matter myelitis is a less severe condition associated with upper motor neuron lesions such as spasticity and hyperreflexia, and has a slower progression of paralysis. TM associated with SLE remains underexplored with an extremely limited number of reported cases. Our patient was referred from a smaller health centre, and as a result of which we lost the initial hours crucial for beginning corticosteroid therapy, as recommended by the EULAR task force. (6) In this study, we provide a case report of a patient with SLE who presented with TM, with an aim to highlight early recognition and prompt treatment with immunosuppressive therapy.
Conclusions: Our report highlights the importance of prompt and aggressive initiation of glucocorticosteroids along with immunosuppressive agents like cyclophosphamide for grey matter myelitis in patients with SLE. The knowledge of the difference between Gray matter and White matter myelitis can aid in diagnosis.