Background: The treatment of acute decompensated heart failure (ADHF) and comorbid acute kidney injury (AKI) can be quite challenging. Many times the etiology of AKI in this setting is multifactorial and may involve cardiorenal syndrome (CRS). Arterial underfilling, sympathetic nervous system upregulation, and systemic venous congestion contribute to impaired glomerular filtration rate in ADHF patients. Our study looked to examine total diuresis achieved in this subgroup of HF patients in regards to percent (%) body weight (BW) reduction, and how it affected early hospital readmission.
Methods: We conducted a retrospective cohort study from July 2014 to June 2015. Data was analyzed from 58 consecutive patients admitted for acute decompensated heart failure with coexisting acute kidney injury (rise in creatinine > 0.3 mg/dL from baseline) in an urban, academic medical center. The primary outcome being measured was difference in mean % reduction in BW (Kg). Reductions in BW were then grouped into < 5%, 5%-10%, and >10%. Secondary measures included the total dose of IV Lasix given throughout hospital stay, B-type natriuretic (BNP) on arrival, admission/peak creatinine, and transition from IV to PO Lasix (days). Patients were divided into 2 groups based on the primary adverse outcome of 30 day hospital readmission. The average for each set of data was compared using a two-sample t-test. A chi-square test was used to compare proportions of BW reductions.
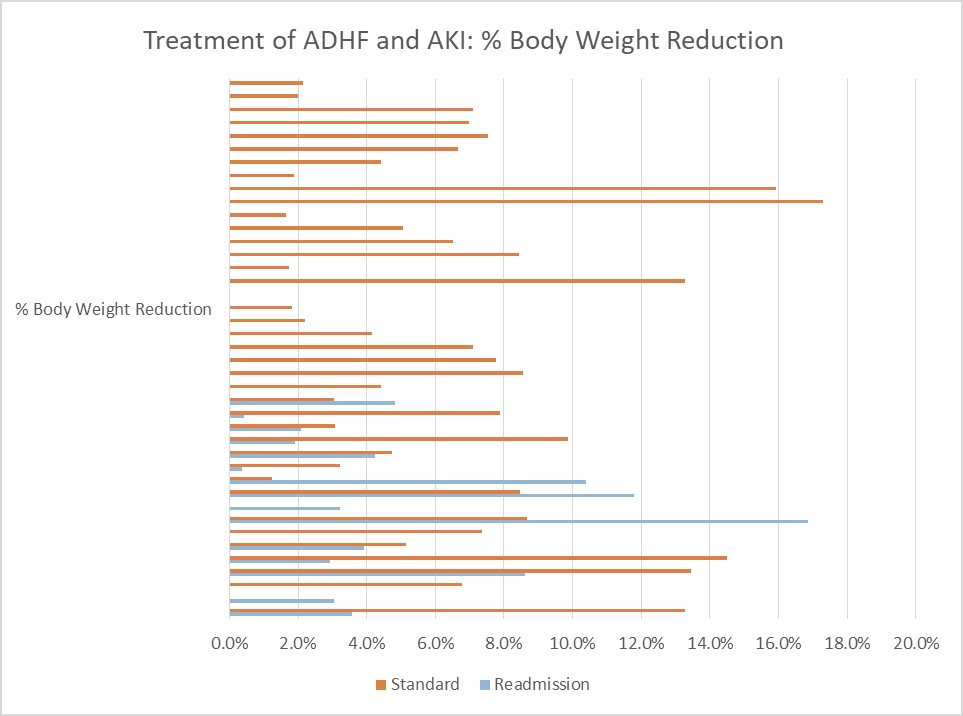
Results: 17 out of 58 patients were readmitted within 30 days of discharge. Readmission group (n=17) vs standard group (n=41): Mean % reduction in body weight (Kg) 4.6% vs 6.2% (Difference: 1.6%, 95% Confidence Interval, 1.57-1.62; p<0.001). Reductions in BW: <5%: 64.7% vs 43.9% (p=0.1); 5%-10%: 5.8% vs 41.4% (p=.008); >10%: 17.6% vs 14.1% (p=0.7).Secondary measures: Admission creatinine (mg/dL) 2.4 vs 1.9 (p=0.09), peak creatinine 2.91 vs 2.33 (p=0.08), total IV Lasix 456mg vs 340mg (p=0.15), transition from IV to PO lasix 1.86 days vs 2.15 days (p=0.64), BNP (pg/mL) 1846 vs 1245 (p=0.07).
Conclusions: Among patients with ADHF and AKI, the mean % reduction in BW was significantly less in those readmitted within 30 days, which was driven by a large disparity in the amount of patients able to achieve 5%-10% reduction in BW. There was a trend toward readmission being associated with higher admission/peak creatinine, higher total lasix IV received, elevated BNP, and shorter transition time from IV to PO lasix in the readmission group.
CRS occurs in approximately 25% of patients admitted with ADHF. Fluid balance in ADHF with AKI is complex with a narrow window for management of both blood pressure and volume. Extremes in either parameter can be associated with worsened renal function. Response to diuretic therapy depends on the severity of AKI and comorbidities. Assessment of intravascular volume and fluid in third spaces, including the abdominal compartment are crucial. If diuresis is suboptimal prior to discharge, early readmission is likely.