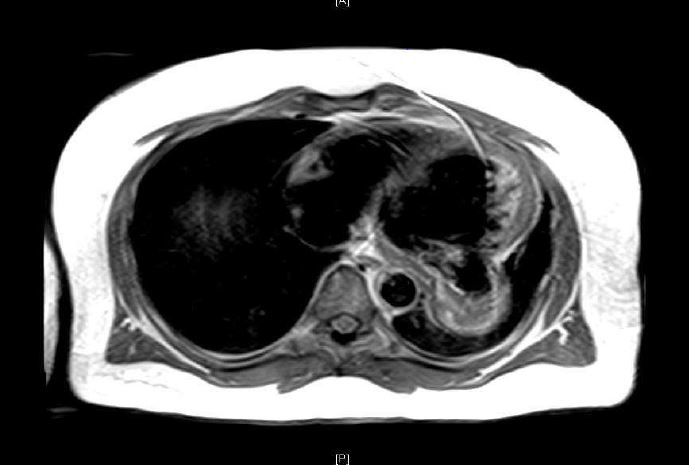
Case Presentation: A 44-year-old man with no known medical conditions presented with acute, painless, left monocular blurred vision. There was no history of smoking or illicit drug use. Physical examination indicated blood pressure of 200/135 mmHg, heart rate 86/min and unremarkable cardiopulmonary exam. Fundoscopic examination showed branched retinal vein occlusion. Patient had elevated Troponin I. Electrocardiogram had pathologic Q-waves in inferolateral leads. Chest X-ray displayed a retro cardiac opacity. Patient was initially managed for hypertensive emergency. Transthoracic echocardiogram (TTE) showed an ejection fraction of 25-30% with dyskinesis and outpouching of basal inferolateral wall concerning for possible pseudoaneurysm with thrombus. A subsequent transesophageal echocardiogram (TEE) confirmed a LV inferolateral PSA with chronic thrombus. Cardiac MRI was remarkable for a 4.6-cm x 6 cm x 5.6 cm PSA with a 3 cm neck and chronic thrombus. Coronary angiography with left ventriculogram showed two-vessel disease (60% proximal LAD and 100% distal RCA) with collaterals and LV outpouching equivocal for pseudo vs true aneurysm. Neck of the aneurysm was not visualized.
Patient was scheduled for surgical resection of PSA. However, intraoperative findings were consistent with true aneurysm as there was no free wall rupture. Successful LV aneurysmal repair with thrombus extraction was done. Patient had a non-complicated post-operative course and is being medically managed now.
Discussion: Free wall rupture of the left ventricle (LV) contained by the adhering pericardium, results in formation of a LV pseudoaneurysm (PSA). A true LV aneurysm, in contrast, is the discrete thinning (<5mm) and resultant outpouching of the ventricular wall. Natural course for pseudoaneurysm is to rupture leading to cardiac tamponade, shock, and death. True aneurysm usually has a benign history, therefore PSA warrants an emergent surgery as compared to an elective surgical repair of aneurysm. Differentiating the two conditions preoperatively, despite the use of various cardiac imaging modalities, remains a challenge to date. We present a case report demonstrating these diagnostic difficulties.
Conclusions: The distinction between true and pseudo LV aneurysm is diagnostically challenging. Both types of aneurysms present with nonspecific symptoms and are mostly incidentally noted on cardiac imaging. When identified, it is important to distinguish accurately between a PSA and true aneurysm given the differing natural history and therapeutic strategies. Echocardiography, left ventriculography and contrast-enhanced cardiac MRI all provide useful information but are not definitive for preoperative diagnosis. Imaging characteristics most suggestive of PSA included a sharp discontinuity of the endocardial border at the base of the pseudoaneurysm, a narrow orifice compared with the aneurysm fundus diameter (Omax/Dmax 0.5 or less) and loss of epicardial fat with blood flow turbulence. Surgical exploration and pathologic assessment is necessary to make a definitive diagnosis.